Allergic rhinitis: from nasal symptoms to accurate diagnosis
Natasha, a 19-year-old healthcare assistant based in Oxford, presents to her GP complaining of nasal congestion, itching, and discharge over the past year. Her symptoms persist throughout each day, causing significant discomfort and difficulty when wearing a mask at work. Over the last few months of summer, the symptoms have worsened slightly, and she has suffered with breathlessness.
Find out how an accurate diagnosis of allergic rhinitis was reached, including allergen sensitisations.
Patient history
Personal history
As an infant, Natasha suffered from egg allergy; however, she can now tolerate egg in baked goods.
Aged 16, Natasha suffered an asthma attack during a sleepover with a friend who had a pet cat. Following this episode, she was diagnosed with asthma by her GP. During the same visit to the GP, it was noted from her medical records that she had suffered with childhood eczema, which gradually improved during her teenage years and had now mostly resolved.
On a previous visit to a dermatologist regarding her eczema, it was found that Natasha has dermatographism.
Medication history
- Previously prescribed intranasal beclomethasone, but stopped due to subsequent epistaxis
- Currently takes inhaled beclomethasone, 200 mcg BD
- Uses intranasal antihistamines and nasal decongestants
Observation
Whilst observing Natasha during the consultation, her GP observed frequent sniffing, nose rubbing, and mouth breathing.
How should Natasha's GP continue the diagnostic workup?
Based on Natasha’s clinical history, a diagnosis of rhinitis may be made. The next step in the diagnostic process is a physical examination, including inspection of the face, and internal examination of the nose. All patients with persistent rhinitis should also be assessed for possible asthma; this should consist of a chest examination, and lung function tests including spirometry or peak flow.1
To determine whether Natasha's rhinitis is allergic or non-allergic in origin, a specific IgE blood test or skin prick test (SPT) should be used. However, in Natasha’s case, SPTs are contraindicated due to her documented dermatographism, making a specific IgE blood test most suitable.1 One study found that compared with a clinical history and physical examination alone, additional use of a specific IgE blood test increases diagnostic certainty by 64 percent.2*
*Based on a prospective multicentre study of 380 children aged <6 years with symptoms of eczema and/or wheezing/asthma and/or rhinitis.2
Examination, investigations, and results
Examination
Natasha’s GP continued the diagnostic process with a physical examination. Inspection of her face was unremarkable, but internal examination of her nose revealed turbinate hypertrophy with clear secretions.
Examination of Natasha’s chest revealed no obvious abnormalities, and chest expansion was equal on both sides. Her respiratory rate was 18 breaths/min, and upon auscultation of her lungs, the GP heard a mild expiratory wheeze.
Investigations
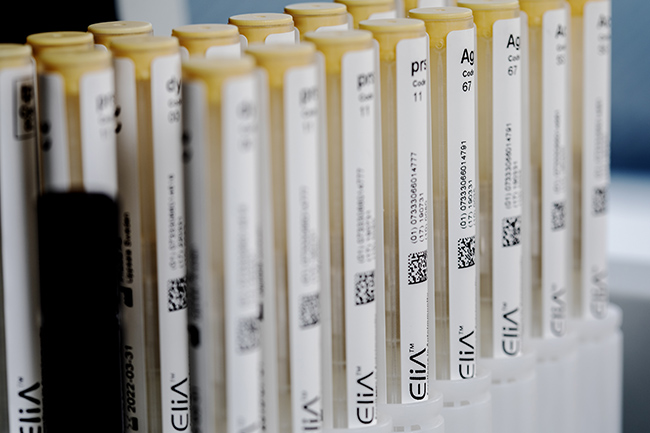
Next, the GP decided to request a specific IgE blood test. Based on Natasha’s symptoms, age, and local sensitisation patterns, an appropriate panel of allergens was selected.
Due to her asthma and worsening breathlessness, Natasha was also referred to an allergy specialist for lung function tests.
Test* |
Type |
Natasha’s Results |
| House dust mite (d1) | Whole allergen |
31 |
| Timothy grass (g6) | Whole allergen |
17 |
Silver birch (t3) |
Whole allergen |
15 |
| Cat dander (e1): | Whole allergen |
<0.10 |
| Alternaria alternata (m6) | Whole allergen |
8 |
Test |
Natasha’s Results |
Peak nasal inspiratory flow |
52 L/min |
Peak expiratory flow rate (PEFR) |
310 L/min |
Percentage of predicted FEV1 |
73 percent |
| Fraction exhaled nitric oxide (FeNO) |
49 ppb |
Differential Diagnosis
What is the most likely reason for Natasha’s nasal symptoms?
Specific IgE blood test results will indicate whether the patient is sensitised (has IgE antibodies) to specific allergens. Specific IgE values of ≥0.10 kUA/L indicate sensitisation,3 and the probability of allergy increases with increasing specific IgE antibody concentrations.4 Results should always be interpreted in conjunction with the clinical history and physical examination.1,5 When test results are concordant with the clinical history, a diagnosis of allergic rhinitis can be made.1
In Natasha’s case, the specific IgE test results show that she is polysensitised, with sensitisations to house dust mite (HDM), Timothy grass, silver birch, and Alternaria alternata. She has very high levels of HDM-specific IgE, but perhaps surprisingly, given her clinical history, her results indicate that she is not sensitised to cat dander. Therefore, it is likely that her asthma attack during the sleepover with her friend was due to HDM rather than the cat—a point which would have been very difficult to ascertain from her history alone.
Natasha’s sensitisation to seasonal allergens (Timothy grass, silver birch, and Alternaria alternata) may be the reason for her worsening nasal symptoms and breathlessness over the summer months, as her total allergen load will be increased compared with winter months.6
Interpreting these results in conjunction with Natasha’s clinical history and physical examination findings, allowed the GP to confirm a diagnosis of IgE-mediated allergy7—in this case, perennial allergic rhinitis (due to HDM) and seasonal allergic rhinitis (due to Timothy grass).
Management
HDMs are impossible to completely eradicate from a house by cleaning;8 however, Natasha could limit her exposure to HDM by using the following strategies:
- Put dust-proof covers on pillows, mattresses, and box springs. Remove and wash the covers frequently.8,9
- Minimise the number of stuffed animals kept in bedrooms or put them in plastic containers.8
- Remove carpets, drapes, and upholstered furniture (as much as possible).9
- Keep humidity to ≤45 percent.9
- Vacuum carpets twice every week.9
Natasha's peak nasal inspiratory flow is below the normal range determined for adult female patients (~115 mL/min), indicating nasal obstruction.10 Normal adult PEFR range is between 400 and 700 L/min.11 From her lung function tests, Natasha's low PEFR and FEV1 suggest intrapulmonary airflow obstruction,12 which, taken together with her clinical history, is indicative of asthma.13 Her FeNO is raised, but caution should be exercised when interpreting this result, as the presence of allergic rhinitis can elevate FeNO levels, even in the absence of overt, clinical asthma.1
Did you know?
- Up to 90 percent of allergic patients are polysensitised.14
- Allergic rhinitis confers a 3.5-fold risk for subsequent development of asthma,15 and is a marker of poor asthma control.16
*The following products are included in the ImmunoCAP™ blood test range:
- ImmunoCAP Allergen d1, House dust mite
- ImmunoCAP Allergen g6, Timothy
- ImmunoCAP Allergen t3, Common silver birch
- ImmunoCAP Allergen e1, Cat dander
- ImmunoCAP Allergen m6, Alternaria alternata
BD : twice a day; FEV1: forced expiratory volume in 1 second; IgE: immunoglobulin E; kUA/L: allergen-specific kilo units per litre
The people, places, and events depicted in these case studies and photographs do not represent actual patients, nor are they affiliated in any way with Thermo Fisher Scientific.
- Scadding G K, Scadding G W. Diagnosing allergic rhinitis. Immunol Allergy Clin North Am 2016;36(2):249-260
- Niggemann B, Nilsson M, Friedrichs F. Paediatric allergy diagnosis in primary care is improved by in vitro allergen-specific IgE testing. Pediatr Allergy Immunol 2008;19(4):325-331
- Popescu F D, Vieru M. Precision medicine allergy immunoassay methods for assessing immunoglobulin E sensitization to aeroallergen molecules. World J Methodol 2018;8(3):17-36
- Soderstrom L, Kober A et al. A further evaluation of the clinical use of specific IgE antibody testing in allergic diseases. Allergy 2003;58(9):921-928
- Bousquet J, Anto J M et al. Allergic rhinitis. Nat Rev Dis Primers 2020;6(1):95
- Matricardi P M, Kleine-Tebbe J et al. EAACI molecular allergology user's guide. Pediatr Allergy Immunol 2016;27 Suppl 23:1-250
- Siles R I, Hsieh F H. Allergy blood testing: a practical guide for clinicians. Cleve Clin J Med 2011;78(9):585-592
- American College of Allergy A I. Environmental trigger avoidance. Available at: https://acaai.org/allergies/allergy-treatment/environmental-trigger-avoidance. Accessed March 2022
- Wilson J M, Platts-Mills T A. Home environmental interventions for house dust mite. J Allergy Clin Immunol Pract 2018;6(1):1-7
- Pellegrino R, Viegi G et al. Interpretative strategies for lung function tests. Eur Respir J 2005;26(5):948-968
- Ottaviano G, Scadding G K et al. Peak nasal inspiratory flow; normal range in adult population. Rhinology 2006;44(1):32-35
- British Lung Foundation. Peak flow test. Available at: https://www.blf.org.uk/support-for-you/breathing-tests/peak-flow. Accessed March 2022
- Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. Available at: https://ginasthma.org/wp-content/uploads/2019/06/GINA-2019-main-report-June-2019-wms.pdf. Accessed March 2022
- Ciprandi G, Alesina R et al. Characteristics of patients with allergic polysensitization: the POLISMAIL study. Eur Ann Allergy Clin Immunol 2008;40(3):77-83
- Shaaban R, Zureik M et al. Rhinitis and onset of asthma: a longitudinal population-based study. Lancet 2008;372(9643):1049-1057
- Thomas M. Allergic rhinitis: evidence for impact on asthma. BMC Pulm Med 2006;6 Suppl 1:S4