Episode 032
Must-Know Tips for Primary Care Managing Food Allergies: Insights from Dr. Ruchi Gupta
-
Summary
-
Episode Resources
-
Transcript
-
Related Episodes
Episode summary
Many of the 33 million Americans affected by food allergies, start their allergy care journey with a visit to their primary care or family medicine clinician. Tune in as Dr. Ruchi Gupta, a board-certified pediatrician and founding director of the Center for Food Allergy and Asthma Research (CFAAR), shares key insights on the current state of food allergies in America as well as impactful diagnostic and management tips that every primary clinician should consider when seeing patients with food allergies.
Guest spotlight

Dr. Ruchi Gupta
Dr. Ruchi Gupta is a distinguished expert in the field of pediatrics and medicine, serving as a professor at Northwestern University Feinberg School of Medicine. With two decades of experience as a board-certified pediatrician, she is the founding director of the Center for Food Allergy and Asthma Research (CFAAR). Dr. Gupta is globally recognized for her pioneering research in food allergy and asthma, contributing significantly to the understanding and management of these conditions. Her work has been instrumental in highlighting the prevalence and public health impact of food allergies, particularly in children, and she continues to advocate for improved diagnostic and management strategies in primary care settings.
Episode resources
Find the resources mentioned in this episode
Lab Ordering Guide
Looking for allergy diagnostic codes from the labs you already use?
Episode transcript
Time stamps
1:26 Dr. Gupta's Journey and Background
3:15 Current State of Food Allergies in America
5:36 Role of Primary Care in Allergy Diagnosis
9:24 Early Introduction of Allergens
12:16 Importance of Allergen Component Testing
16:47 Building a Collaborative Care Team
21:30 Ideal Management of Food Allergies in Primary Care
Announcer:
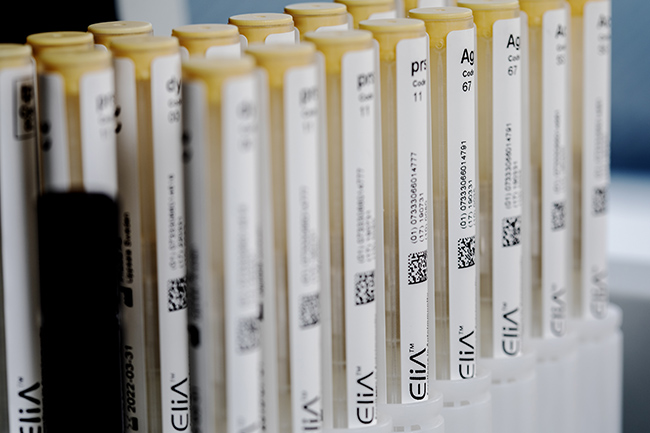
Announcer [00:00:00]: ImmunoCAST is brought to you by Thermo Fisher Scientific, creators of ImmunoCAP Specific IgE diagnostics and Phadia Laboratory systems.
Gary Falcetano [00:00:12]: I'm Gary Falcetano, a licensed and board certified PA with over 12 years experience in allergy and immunology.
Luke Lemons [00:00:19]: And I'm Luke lemons, with over 6 years experience writing for healthcare providers and educating on allergies. You're listening to ImmunoCast, your source for medically and scientifically backed allergy insights. Hi, welcome to immunocast. We are here at the American Academy of Asthma, Allergy and Immunology, a joint conference with the World Allergy Organization. And Gary and I are really excited. We're sitting down with the incredible Dr. Ruchi Gupta.
Gary Falcetano [00:00:46]: The famous Ruchi Gupta. Yes. So Ruchi is a professor of pediatrics and medicine, Northwestern University Feinberg School of Medicine, attending physician with 20 years of experience as a board certified pediatrician, founding director of the center for Food Allergy and Asthma Research, cifar, and world renowned for her groundbreaking research in the areas of food allergy and asthma. So welcome Ruchi. We're really excited to have you here today.
Dr. Gupta [00:01:12]: Well, thank you so much. I'm excited to be here.
Luke Lemons [00:01:15]: Yeah. So, I mean, Gary just rambled off a laundry list. You are very, very, very well versed in food allergy and pediatrics. And can you start by sharing a little bit about your journey and your background to get where you are now?
Dr. Gupta [00:01:26]: Sure, absolutely. So I started out in Louisville, Kentucky, if you want to go back that far.
Gary Falcetano [00:01:32]: I didn't realize that.
Dr. Gupta [00:01:33]: Yeah, I'm from Louisville. I went to med school there and then did my residency in Seattle, PEDs residency in Seattle and then went from there, which was an amazing program. And then went to Boston and got my Master's of Public health at the Harvard School of Public Health. And I did a fellowship at Boston Children's and then landed in Chicago. And, and originally I was very interested in studying asthma disparities and so went to Chicago to work with world renown asthma researcher and interestingly met a family who had two young children with food allergies. And this is 20 some years ago now, 20, 21, 22 years ago. And their story was just so inspiring because they were talking so much about their two kids with food allergies. And back then we really didn't understand food allerg. We just knew there was something happening in this big rise. So it really got me thinking and thought I could use my newfound skills and my MPH to really look into this area that had so many holes compared to asthma. So I got started, and one of our first tasks was to really understand the prevalence, like the public health impact, what's happening with food allergy. And that is, you know, what really got me into this field, because we found that 8% of kids have food allergy. And that number was so staggering back then. You know, that's 1 in 13 kids. And then we were able to characterize the types of foods they were allergic to, which had been done, and severity and so many other things. So that was my beginning of my journey.
Gary Falcetano [00:03:15]: Since then, you've published multiple papers on prevalence, on the epidemiology of food allergy. What can you tell us now about the current state of food allergy in America?
Dr. Gupta [00:03:25]: Yeah, so food allergies are a big deal. So I would even call it an epidemic.
Gary Falcetano [00:03:30]: 33 million by some estimates.
Dr. Gupta [00:03:32]: 33 million, that's exactly right. And so what's really interesting is we know, you know, we published all that data on kids, and then being a pediatrician, I didn't really think about adults, but all those kids turn into adults. And so people started asking, like, what about the adult population? And so we did do a study on adults. And that was just fascinating, very unexpected. You know, what we found is that 1 in 10 adults have a convincing food allergy. But what's really interesting about that is one in five adults checked, yes, I have a food allergy. So if you self reported about 1 in 5, 20% of adults in America are avoiding a food because they think they have a food allergy. All right, now how many do you think actually went to a physician to get it diagnosed out of the.
Luke Lemons [00:04:26]: I'm gonna say 10% of those?
Dr. Gupta [00:04:28]: 1 in 20.
Luke Lemons [00:04:30]: Wow.
Dr. Gupta [00:04:31]: 5%. And it makes sense. I mean, really, I'm an adult, and I don't want you to guess how many years it's been since I've been to a doctor. But we take care of our kids so much better than we take care of ourselves. And I think that was very eye opening in terms of it is a big problem. And even if you think of it as, okay, 1 in 10 adults, that adds up to the 33 million with the kids. But if you think that even more than that, double that are avoiding foods because they think they have a food allergy, then so many Americans are avoiding something because of this perceived allergy and understanding the difference between allergies and intolerances and celiac and I mean, there's so many things that food can cause, and.
Gary Falcetano [00:05:16]: There'S lots of Things that make us feel bad. Right. When we eat foods. But they're not all allergy.
Dr. Gupta [00:05:20]: Exactly.
Gary Falcetano [00:05:21]: Can you speak to being a pediatrician, not an allergist?
Dr. Gupta [00:05:24]: Yes.
Gary Falcetano [00:05:24]: Speak to pediatricians or family practice providers, role in getting those. All of those adults and children. Right. That think they have allergy, getting them to the right diagnosis.
Dr. Gupta [00:05:36]: Oh, my goodness. This is something I am so passionate about because pediatricians are frontline. Right. They are the ones seeing everyone. And it is so critical that they are able to identify food allergies and manage it to some degree and give them what they need, their epinephrine, their action plan. And it is challenging for them because they don't usually do the testing. And so then they refer to an allergist. But one of the biggest, biggest issues we're having is access to care because there are not that many allergies.
Gary Falcetano [00:06:13]: I think 5,000 by some estimates, of clinically practicing, right?
Dr. Gupta [00:06:17]: Yeah, yeah. All right, so 5,000 clinically practicing, but only about. I think the number is 4,000 C food allergy. And of that 4,000 a study we just did, only half of them take Medicaid.
Gary Falcetano [00:06:31]: That's major access issues.
Dr. Gupta [00:06:32]: Yeah, yeah. So we mapped it, and if you look across the country, there are major holes in rural areas and certain states. And then what do those kids do? And how do you get 33 million to 4,000 allergists across the country and then especially the underserved population, and it.
Luke Lemons [00:06:50]: Just goes back again to the primary care provider, like who's there and the pediatrician, because they are often the first stop that those children are going to visit in their. In their healthcare journey.
Dr. Gupta [00:07:00]: Right. And sometimes the only stop.
Luke Lemons [00:07:02]: Yes. And so when it comes to the role of, let's say, diagnostic testing for these primary care clinicians, let's say that I am a practicing pediatrician in an area that doesn't have access to an allergist. How can I best equip my practice to serve this community?
Dr. Gupta [00:07:17]: Right. That is a really important question. And how do we get them comfortable diagnosing it? So what we talk about is take a really good history. Right. Ask the right questions. What food was it that was new, that caused the reaction? What kind of a reaction did they have? Did they have typical food allergy, allergic reaction symptoms? A lot of times vomiting happens in food allergy, but also in food poisoning and many other things, GI conditions. So really teasing it apart, being very diligent about that. And then in terms of testing, if they really do feel okay, it was the first time they had A cashew and they broke out into hives and they vomited and kind of felt dizzy. Pretty clear. So then what do you do? So another thing you can do is test. And now pediatricians don't tend to have the ability to do skin prick tests in their eyes office, but they do blood work. So how do we educate them on what kind of testing they can do, you know, specific iges to the food? What happened was pediatricians started doing panel testing and then everyone was like, no, no, because you're cutting out food. But it is not difficult for pediatricians to learn what specific iges to order for the food that may be the culprit.
Gary Falcetano [00:08:36]: Exactly. And the interpretation side of that is the most important. Right. Because you can get test results, but knowing what to do with not to cut out foods necessarily that are not culprits and really how to manage in their practice and then potentially refer, if you have that ability, right. To the food allergy allergist.
Dr. Gupta [00:08:54]: And, you know, if the allergist. What I'm hoping for is we can have some kind of communication telehealth, something where they can communicate with the allergist and let them know. Now, we do a lot with prevention, and if it's a high risk kid with severe eczema, we do encourage that pediatrician to get a specific ige to peanut immediately, because if it's negative, the negative predictive value is so high. Tell them to go ahead and eat. You know, if they're scared and you don't need the allergist because that's gonna.
Gary Falcetano [00:09:24]: Take additional time and we could close that window. So you know what, why don't you talk a little bit about that? Because I think we tend to think that this has been out there, what, since 2017, 2018.
Dr. Gupta [00:09:35]: Yeah.
Gary Falcetano [00:09:36]: But it's still so underutilized, the early feeding. Right. To prevent allerg. So maybe take a minute and talk about that.
Dr. Gupta [00:09:42]: Sure. So, you know, this is totally pediatricians right here. So pediatricians are seeing those babies and.
Gary Falcetano [00:09:49]: Family practice that are seeing these.
Dr. Gupta [00:09:50]: Sorry, yes.
Gary Falcetano [00:09:50]: Can't forget about a lot of the rural areas.
Dr. Gupta [00:09:52]: Right? Oh, no. A family practice is so important. And you know, when you talk about that, PAs and nurse practitioners, like these amazing clinicians, you know, hundreds of millions of patients Right. Everywhere, all over. They're the first line. And so what we know now is early introduction can actually prevent food allergy from developing. And this is a lot of research we're doing in our lab. And having that physician recommend it early is critical to that family starting to eat those foods. And we're going to be present. Actually, that's what we're Presenting today at 2 is our results. Because we helped pediatricians and family practice encourage parents, we put it into their EMRs, into their, well, child care notes, templates and them encouraging families increased the amount of families that actually did introduce effectively. And so it does work.
Gary Falcetano [00:10:47]: Their word does hold some weight. Right.
Dr. Gupta [00:10:50]: So much. And so we need the pediatrician to recommend it. But the controversy right now is what about these high risk kids? Because the original NIAID guidelines said if you are high risk, which means severe eczema, then you need to go to an allergist immediately and get tested because you're at the highest risk. Now what we found is that step takes so long that like you said, you're losing time and you could be causing the allergy.
Gary Falcetano [00:11:18]: Because we know the earlier you introduce, the more effective it is in prevention.
Dr. Gupta [00:11:21]: That is exactly right. So what we would love for pediatricians to do is either just have them introduce if they're comfortable, but a lot of families aren't. So then the next thing that they can do immediately is get that specific ige to peanut and that test will come back in a day. And then they have a number and that number is so reliable. And if it is over a 0.35, send them to the allergist, but call that allergist and get them in immediately. And if it's under eat immediately.
Gary Falcetano [00:11:52]: Right.
Dr. Gupta [00:11:52]: Just start that fiat.
Luke Lemons [00:11:54]: And it's also, I mean, looking at allergen components too, that sort of testing when it comes to specific iGen can even further build out the referral process and the understanding. And you had mentioned interpretation earlier and we do have resources for that in this episode's description. If you click the link, we'll have all the food interpretation guides. But can you talk about the role of allergen components also in that?
Dr. Gupta [00:12:16]: Absolutely. I mean, allergen components just make it that much more reliable. Right. They are so powerful. And if you can order components, you must. And so how do we get that education to pediatricians? Because if they could get component testing on any of the foods that they are suspecting, they could have reliable answers immediately to help that family manage that allergy.
Gary Falcetano [00:12:40]: And in a lot of laboratories they are able to order with a reflex, so it doesn't go to the components unless the whole allergen is positive. But then when they get that information, as you said, it provides so much more information to really kind of. We know that whole extract testing, especially for peanut is very sensitive, as you said. Right. It rules out if it's negative, but when it's positive, it may not be a true clinical positive or allergy. Right. And that's where the components come in.
Dr. Gupta [00:13:06]: Making sure pediatricians have education on that and access to components. And if we can make that happen, I think it is going to be a complete game changer because there are so many kids we see. So when we looked at even kids in our prevalence study, we say 8% of kids have food allergy, but only 5% of them are being diagnosed. So there is still that 3%, which is a lot. They're not getting to an allergist, but they have symptoms of a true convincing food allergy. And we know this, like we said, with only 4,000 allergists seeing food allergies.
Gary Falcetano [00:13:42]: How could they possibly have to get to. Exactly.
Dr. Gupta [00:13:45]: And I mean, we're doing studies looking at wait time. And even if you have insurance, wait time can be so long. You know, at our hospital, wait time to see an allergist is nine months. And that's with insurance. You know, so again, there's so many access issues in the way that if that primary care provider could actually take on. And it's, I think about it, it's so similar to what we do in asthma. Right. So same thing. The pediatrician, the primary care provider, the family practice doctor, their first line. And they know how to manage asthma to a certain level. And then if it gets too severe, too challenging, then they refer. Exactly.
Gary Falcetano [00:14:25]: Pulmonology, stepwise, NIH approach.
Dr. Gupta [00:14:27]: Right, Exactly. And that's what we really need to get out for primary care providers. And they want it. They're interested because they're observing this. I get so many of them calling me, saying, can you help me get this kid in? Right. And so how do you do that? You make phone calls, but it's not practical.
Luke Lemons [00:14:44]: You have to learn up. You have to educate and know your options when these patients do come in.
Gary Falcetano [00:14:48]: And empowering primary care to really do that, to practice to their full scope.
Dr. Gupta [00:14:54]: Yes. And primary care providers, oh my God, they are the most brilliant people ever.
Gary Falcetano [00:14:58]: Exactly. I've heard allergists say, I really don't want. They have difficulty with interpretation of food allergy testing. And I kind of look at them and I say, you do know they interpret things like thyroid function tests. Right. So with a little guidance, a little bit of self learning, this is something that every primary care provider can do.
Luke Lemons [00:15:19]: This is so valuable. You had mentioned earlier the issue about getting being covered even I think in one of your papers that you had mentioned, only 55% of allergists will take Medicaid. And so a lot of primary care providers are in a position to help those patients who are in need of healthcare.
Dr. Gupta [00:15:35]: Right. And, you know, as I've been in this space, as a pediatrician in an allergy world for 20 years, finally, I feel like the allergist is like, okay, okay, take the rural patients, take the Medicaid patients. We just cannot get to them. You know, take as many of those. No one is going to be out of a job.
Gary Falcetano [00:15:52]: No, no. And, you know, the flip side of that is we can't really blame our allergist colleagues. Right. We all need to work together to improve reimbursements and coverages and stuff. So it is a multifactorial kind of issue, for sure.
Dr. Gupta [00:16:05]: Absolutely. And I think with technology now, they can help with consults, with the pediatrician, they can work hand in hand, but the pediatric provider can manage with assistance. You know, and so we gotta build those systems now. You know, it can't just be a visit. It can be, all right, I'm gonna consult this allergist, make sure everything I'm doing is per protocol, and then move forward, and they'll get more and more comfortable with it. Like you said, I go to clinic, I tell you, like, allergy is the easiest thing ever compared to everything they're doing. And so this is not hard to teach. It's a simple test, It's a simple result. It's very straightforward. Yeah.
Luke Lemons [00:16:47]: We had interviewed Dr. Rubin, who's a big social media guy, and one of his. At the end of the podcast, his advice was as an allergist or as a primary care clinician. Reach out to your local allergist, see if they're willing to come in, see if they're willing to talk. There should be a real bond between primary care and pediatricians, family medicine. And the allergist, being that we do have. What'd you say, 33 million patients with food allergy out there. It's a team effort.
Gary Falcetano [00:17:13]: Yeah. And, you know, speaking of teams, Luke maybe speak to. It's not just the primary care providers and the allergists, but dietitians and psychologists. Exactly.
Luke Lemons [00:17:23]: Right.
Dr. Gupta [00:17:23]: I mean, food allergy is complex. Right. Because food is a part of everything we do. And so you're talking about that kid who has to watch every meal, every morsel they put in their mouth. And I don't know if I mentioned it, but my own daughter has food allergies so, yeah. So it was interesting because as I started in the field of food allergy, I had a son who has no food allergies. And then my daughter was born and he's eating his PB and J and playing with my daughter and gets some in her mouth and I hear screams and she breaks out in hives and is vomiting and. And then I became a mom of a kid with food allergy. I started living it in my own life. And then I was locked in. I'm like, this is it. And so you know what's been interesting? I wouldn't wish it on anyone, but it is eye opening to see how much it impacts absolutely everything you do. And having a kid with it and without it is also really interesting because don't worry about him at all. You know, go wherever, eat whatever. And with her, it's every single thing. You know, going to school, going to play dates, you know, meeting your friends. And then as she became a teenager, going out alone, wanting to go to parties.
Gary Falcetano [00:18:36]: Those life transitions, right? Yeah.
Dr. Gupta [00:18:39]: And now she's in college and that transition was also challenging. You know, now you're going to be completely independent. I know you're going to be at all kinds of social things. So as I progressed in my research career, I really took that into account. And so having access to like, dietitians. Right. So what diets can you have? Because I can even tell you, even for my daughter, who has peanuts, tree nuts, so it's not as complicated as some other kids. With so many others, like milk and egg and wheat and soy, what was really interesting is she still had a very limited diet. Like we would have Italian or Mexican because those are two that you were sure of. We couldn't even really have Indian food unless I made it. And I don't really cook that much, but I did for her. But it is really limiting. So we didn't get to explore different cuisines and food. It's, do you live to eat or eat to live?
Gary Falcetano [00:19:32]: Exactly. Right. It's not just nutrition. It can be an integral part of life.
Dr. Gupta [00:19:36]: Right? Yeah, yeah. So that she definitely ate to live, and my son definitely lived to eat. So it's just so much. And so having access to dietitians and to psychologists to really help you, and then you. You go through so many challenges. Right. So there was a time we took all the foods out of our house and then we were at like social events and someone would bring in like walnut brownies and she would be so scared and she would want to leave right away. And how do you take that fear away that you can be in the same room?
Gary Falcetano [00:20:08]: Exactly. You can be in control, right? Yes.
Dr. Gupta [00:20:10]: And, and so, you know, learning so many things, role playing with people who are pressuring you, you know, so I try to incorporate that into my research a lot. And we've done a lot of quality of life studies as well and tried to build in things to support families and to support pediatricians. You know, we have a conference every summer. We're going to have it this summer. We want to bring pediatricians and we have travel grants from rural areas, from FQHCs to really learn to manage Right. And build those partnerships.
Gary Falcetano [00:20:40]: And we'll, we'll put a link in the, in the show notes for that as well.
Dr. Gupta [00:20:44]: Please do. Because my ultimate goal is to help primary care really understand and manage, you know, food allergies and work together with allergists to make that happen.
Luke Lemons [00:20:56]: Yeah, it's, it's building out that team. Everybody has a special role on that team. And if it's primary care, it's getting those results, looking at history, diagnosing and then evaluating do they need to have counseling? How can we help build the other half of health? The other, there's physical health, there's mental health. We can't forget about the other half. But I wanted to ask you, in an ideal world, how would primary care diagnose and manage patients with suspected food allergies? And what is your take home message to any clinicians who are listening who maybe have some experience with food allergies or have none at all?
Dr. Gupta [00:21:30]: Yes. And you know, I made a music video on this.
Luke Lemons [00:21:32]: I'm glad you mentioned it. We were trying to figure out how to bring it up.
Gary Falcetano [00:21:35]: I, I love that video. Oh my goodness, it's amazing.
Luke Lemons [00:21:39]: We'll talk if we want to put that link in the description.
Gary Falcetano [00:21:42]: You let us know if you're okay with it. We'll definitely do it.
Luke Lemons [00:21:45]: It was great.
Dr. Gupta [00:21:46]: I mean, that's the reason I made it right. Is to help primary care physicians know what to do, how to diagnose and manage. So it's five steps, pretty simple. Step one, you know, take a good clinical history. Right. So make sure you know what foods and what symptoms and try to match them up as best as possible. And step two, even there, I said get a specific ige. So get it, you know, it's not going to hurt and it can only help. And if they get into the allergist beforehand, the allergist will have that data. So order a specific IGE to The foods in question. And then the third is order. Give them a action plan. You know, an anaphylaxis action plan. Very, very important for them in school to know what to do if they have an allergic reaction. And then prescribe epinephrine and then refer to an allergist. You know, so those are five easy steps for primary care on what to do.
Gary Falcetano [00:22:38]: And once you hear the song, you'll never forget them.
Luke Lemons [00:22:40]: Yeah, it's just for those who are curious listening. It's called I Will Thrive. Right. And it's to I will survive. It's great, it's great, it's great. But that's a great message to bring home to those clinicians, because food allergy is, like you said, it's everywhere right now. And we just have to be sure that we're protecting our patients and setting them best up in the future.
Dr. Gupta [00:23:01]: You know, in an example I'll give you, we did a study in the Medicaid population, and if you look at diagnoses codes in Medicaid, asthma is what it is normally, because pediatricians do diagnose asthma. So I think it was like 9% asthma. Atopic derm was normal. And then food allergies was 0.6%.6.
Luke Lemons [00:23:25]: Wow.
Gary Falcetano [00:23:26]: Mortally under diagnosed.
Dr. Gupta [00:23:29]: Yes. Because they're boring. And pediatricians at primary care are not comfortable putting the diagnosis in before they go to the allergist. And so the big thing I will encourage, when you do those five steps, put in the diagnosis, don't do the diagnosis.
Gary Falcetano [00:23:44]: You're not gonna do the accurate treatment. Right. And that's.
Dr. Gupta [00:23:47]: Right. And then, you know, you see these numbers. I mean, 0.6% when we know it's 8%. Yeah.
Gary Falcetano [00:23:55]: And higher in some populations. Right. Yeah.
Dr. Gupta [00:23:57]: Yeah. So that just, you know, takes it home. We really need to at least put in the diagnosis, do those five steps, make sure they're managed well. And, you know, now we need to talk to them about treatments, and we need to talk to them about prevention. So it's really hitting home for the primary care providers.
Luke Lemons [00:24:14]: Yeah. And we have all those resources as well in the link in the description of this episode. From interpretation guides to ways that you can help best manage patience. It's such an important cause. And we want to thank you so much for coming here on immunocast today and sharing all this information. We hope that everybody who's listening also enjoyed it as well. Gary, I don't know if you have any closing questions.
Gary Falcetano [00:24:35]: I just want to thank you again. I'm glad we finally got a chance to sit down and I want to thank everyone out there and, you know, thanks for listening and we'll see you next time.
Luke Lemons [00:24:43]: Thank you.
Dr. Gupta [00:24:44]: Thank you.
Announcer [00:24:50]: ImmunoCAST is brought to you by Thermo Fisher Scientific, creators of ImmunoCAP Specific IgE diagnostics and Phadia Laboratory Systems. For more information on allergies and Specific IgE testing, please visit thermofisher.com. ImmunoCAP Specific IgE testing is an aid to healthcare providers in the diagnosis of allergy and cannot alone diagnose a clinical allergy. Clinical history alongside specific IGE testing is needed to diagnose a clinical allergy. The content of this podcast is not intended to be and should not be interpreted as, or substitute professional medical advice, diagnosis or treatment. Any medical questions pertaining to one's own health should be discussed with a healthcare provider.
- Golden DBK. et al. Anaphylaxis: A 2023 practice parameter update. Ann Allergy Asthma Immunol. 2024 Feb;132(2):124-176.
- Spillner E, Blank S, Jakob T. Hymenoptera allergens: from venom to "venome". Front Immunol. 2014 Feb 28;5:77.
- Blank S, Grosch J, Ollert M, Bilò MB. Precision Medicine in Hymenoptera Venom Allergy: Diagnostics, Biomarkers, and Therapy of Different Endotypes and Phenotypes. Front Immunol. 2020 Oct 22;11:579409.
- Golden DB, Marsh DG, Kagey-Sobotka A, Freidhoff L, Szklo M, Valentine MD, Lichtenstein LM. Epidemiology of insect venom sensitivity. JAMA. 1989 Jul 14;262(2):240-4.
- Ellis AK, Casale TB, Kaliner M, Oppenheimer J, Spergel JM, Fleischer DM, Bernstein D, Camargo CA Jr, Lowenthal R, Tanimoto S. Development of neffy, an Epinephrine Nasal Spray, for Severe Allergic Reactions. Pharmaceutics. 2024 Jun 14;16(6):811.

Legal manufacturer: Phadia AB.
Before you proceed ...
We noticed you may be visiting a version of our website that doesn’t match your current location. Would you like to view content based on your region?
Talk with us
Interested in utilizing our solutions in your laboratory or healthcare practice?
This form is dedicated to healthcare and laboratory professionals who work within medical laboratories, private practices, health systems, and the like.
By clicking "continue with form" you are confirming that you work within a healthcare or laboratory space.
Not a lab professional or clinician but interested in diagnostic testing for allergies?
Visit Allergy InsiderChoose your preferred language
Please note: By selecting a different language, you are choosing to view another site. Product availability and indications may vary from what is approved in your region.