Episode 030
From Pollen to Plate: Understanding Pollen Food Allergy Syndrome
-
Summary
-
Episode Resources
-
Transcript
-
Related Episodes
Episode summary
This spring, patients may be reporting that some foods cause their mouth to itch. Is this a food allergy? Or is this pollen food allergy syndrome (PFAS)? In this episode of ImmunoCAST tackles the clinical challenge of distinguishing this condition from more severe food allergies. We explore the mechanisms behind PFAS, its relationship to seasonal allergies, and the importance of comprehensive allergy evaluation. Key topics include the role of specific IgE testing, differentiating between true food allergies and cross-reactivity with pollen, and management strategies such as avoiding trigger foods and processing methods to denature allergens. Gain valuable insights into improving patient outcomes through accurate diagnosis and tailored management plans.
Episode resources
Find the resources mentioned in this episode
Lab Ordering Guide
Looking for allergy diagnostic codes from the labs you already use?
Episode transcript
Time stamps
1:00-2:08 - Defining Pollen Food Allergy Syndrome
2:25-3:32 - Mechanism of Pollen Food Allergy Syndrome
3:49-5:30 - Rare Systemic Reactions
5:30-6:30 - Common Food Triggers
6:43-8:36 - Clinical Presentation and Diagnosis
8:48-10:28 - Importance of Allergen Component Testing
10:28-12:21 - Differentiating from Severe Food Allergies
12:36-14:42 - Management Strategies
15:34-17:04 - Spring Allergy Considerations
Announcer:
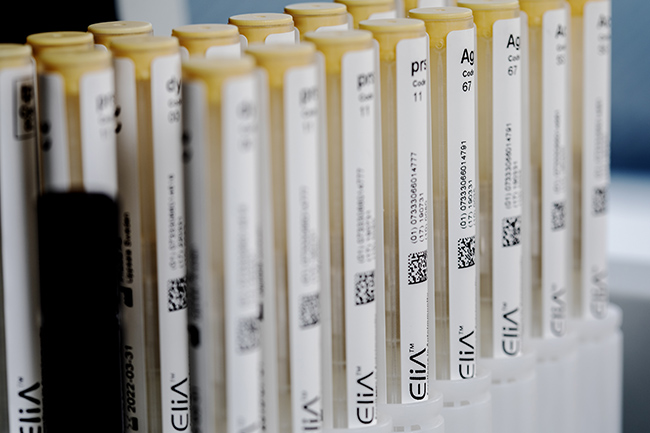
ImmunoCAST is brought to you by ImmunoCAPTM Specific IgE testing and PhadiaTM Laboratory Systems, products of Thermo Fisher Scientific. The content of this podcast is not intended to be and should not be interpreted as a substitute for professional medical advice, diagnosis, or treatment. For patients any medical questions pertaining to one's own health should be discussed with a healthcare provider.
Gary Falcetano (00:13):
I'm Gary Falcetano, a licensed and board certified PA with over 12 years experience in allergy and immunology.
Luke Lemons (00:19):
And I'm Luke Lemons with over six years experience writing for healthcare providers and educating on allergies. You're listening to cast your source for medically and scientifically backed allergy insights. Hi. Welcome to Immuno Cast. We are on location at the American Academy of Asthma Allergy and Immunology. It's a joint conference with the World Allergy Organization. So if you hear any background noise, it's probably all the people on the conference floor also heading around learning about allergies.
Gary Falcetano (00:47):
They're really excited about allergy
Luke Lemons (00:48):
And we are too. We're really excited about allergy. But we wanted to bring this episode to you, especially around springtime to discuss something that is maybe a little bit different than respiratory allergies and pollen allergy.
Gary Falcetano (01:00):
Right? Because this time of year, that's what's top of mind, right? Pollen allergies, a lot of respiratory symptoms, but there's some related conditions to those pollen allergies. So we want to talk about those today as well.
Luke Lemons (01:12):
And we're talking specifically about pollen food allergy syndrome
Gary Falcetano (01:16):
Or what used to be known as oral allergy syndrome.
Luke Lemons (01:19):
Yes. And so this is a syndrome that some of your patients may have experienced where their mouth kind of itches after eating certain foods or certain fruits or other plant foods. It can cause their throat to itch. It can cause their tongue to itch
Gary Falcetano (01:34):
Some swelling of the oropharynx.
Luke Lemons (01:36):
Yes. And so you would assume, oh, why isn't it called oral allergy syndrome anymore?
Gary Falcetano (01:41):
Yeah, well, so it certainly is that constellation of symptoms right in the upper airway and upper esophagus. But it's not just the oral cavity. We can also have some lower symptoms. And in rare instances, this pollen food allergy syndrome, which is now what we're calling it, can actually end up with a systemic reaction. Pretty rare, but it can happen. So we want to make sure that we have a bit better accurate or more accurate description of exactly what this is.
Luke Lemons (02:08):
And it's not uncommon in children we see up to 20% of children will have this syndrome and then up to 58% of adults. And it could be, for example, taking a bite of an apple and the back of the throat feels a little itchy. I know for me, when I eat bananas, I get that exact syndrome.
Gary Falcetano (02:25):
Exactly. And those prevalence numbers do vary pretty widely. And what they found is that we see higher levels in areas of the country where there's a lot more of certain pollens like tree pollens, birch pollens. So the northeast, those prevalence numbers are a little bit higher than some of the other areas.
Luke Lemons (02:43):
And so why don't we go into that? Why does this exist? Technically, it kind is like a food allergy, but yeah, it's a food allergy, but it's related to pollen. So why is that, Gary?
Gary Falcetano (02:52):
Exactly. So when we're allergic to pollen and we have respiratory symptoms, there's certain proteins, and we've talked about this on numerous other episodes, there's certain proteins that you develop antibodies to and they cause the respiratory symptoms when you're exposed to those allergens in certain plant foods, there's similar looking proteins. So they have similar amino acid sequences to the pollens. And what happens is your body recognizes those proteins in the plant foods and it thinks they are almost identical, but it thinks they're the same allergen as the pollens. So your body reacts to it, but this time, because you ingested it, you have food-like symptoms as opposed to respiratory symptoms.
Luke Lemons (03:33):
And we want to say also your patients who may experience this, those proteins that are similar, they often get denatured in the digestion track, which is different from a lipid transfer protein, which is associated with more severe food allergy syndromes.
Gary Falcetano (03:49):
Exactly. We can get some oral symptoms from lipid transfer proteins. We can get them from, if you remember back to our Trina peanut episode, the storage proteins, which are synonymous with more systemic type reactivity. We can still have those oral symptoms along with systemic symptoms for some of the proteins. But the proteins that are really responsible for the food pollen allergy syndrome are those labile proteins, those ones that typically get denatured either by digestion in the gut or by heating or sometimes peeling like a fruit because some of those allergens are concentrated in the peel.
Luke Lemons (04:23):
And you had mentioned earlier that it's rare to have a systemic reaction if you have pollen food allergy syndrome.
Gary Falcetano (04:29):
Exactly.
Luke Lemons (04:29):
So what are the exceptions to that? What does systemic reaction happen?
Gary Falcetano (04:33):
Yeah, so there's been cases in the literature that really speak to really overwhelming your body's ability to denature the protein. One case study I'm familiar with was an adolescent female had food pollen allergy syndrome to peanuts, but one day was exercise in police. She was playing soccer game, ate a whole lot of peanuts after the soccer game almost immediately after a lot of peanuts. And so her body couldn't denature all of that protein
Luke Lemons (05:00):
Overwhelm the
Gary Falcetano (05:00):
System and exercise. We've talked about co-factors in the past, combining exercise with that, she had a systemic reaction. And when they tested her, and we talk about with peanuts, we talk about some of those allergen components, high risk, low risk. She was only ariah eight, which is the birch pollen homologous protein.
Luke Lemons (05:19):
Yeah, that's what the activity is.
Gary Falcetano (05:21):
But she definitely had a systemic reaction. And some of the reports in literature up to 1%, 1.7% in some cases of food pollen syndrome can actually result in systemic reactions.
Luke Lemons (05:30):
Wow. Well, I mean, why don't we talk a little bit about, you mentioned the birch pollen for the peanut allergy, but let's also name off of some other foods that are associated with that. So with birch, pollen, others, apple, almond, carrot, celery, hazelnut, kiwi, peach, pear, plum, all those stone fruits
Gary Falcetano (05:48):
Sounds like a great platter,
Luke Lemons (05:49):
But not if you have fallen food allergies, your mouth uncomfortable, the grass pollen also.
Gary Falcetano (05:54):
Right there we see things like melons, peaches, tomatoes,
Luke Lemons (05:59):
And then ragweed. We see banana cucumber, which I have ragweed, which is why I have that syndrome. And then
Gary Falcetano (06:04):
And melon,
Luke Lemons (06:04):
Melon,
Gary Falcetano (06:04):
Melon air. I think that's the one we think about a lot. We hear a lot about ragweed, melon syndrome.
Luke Lemons (06:09):
Yes. Yeah. This isn't the only disease state that has relationship with fruit too. And maybe in another episode we talk about the relationship between kiwi and latex. And I'm curious, does that also have to do with a plant protein
Gary Falcetano (06:21):
That does, because latex is a plant, right? Latex from the rubber plant. Right. And so it contains proteins that are very similar to those found in banana and kiwi.
Luke Lemons (06:31):
And so we've spent a lot of time, I guess, dissecting what pollen food allergy syndrome is and the things that can cause it. Why don't we go into a clinical presentation and a diagnosis of this disease statement that's important.
Gary Falcetano (06:43):
Sure. So I think go back to that adolescent female, a 16-year-old presents after eating some peanuts, having oral itching, maybe a little tongue swelling. Pretty sure it was the peanut. There was no other foods involved at the time. Close proximity time too. Yeah, exactly. And this did happen in the spring, so we always go to history first. So in taking the history, we find that out, the immediate history of that reaction, but also that she has symptoms in the springtime and maybe in the summer as well that seem to be seasonal allergy related respiratory symptoms along with these kind of localized mouth symptoms when she ate the peanut.
Luke Lemons (07:23):
So she comes into the office and the clinician looks at that history. First thing, if they're having respiratory symptoms, it's probably good to evaluate them for a respiratory allergy.
Gary Falcetano (07:33):
It is, right. But she presents with kind of a food symptom.
Luke Lemons (07:37):
Yes.
Gary Falcetano (07:37):
So maybe we want to kind of address the food first, or maybe we do them. Let's talk about the food and then maybe let, we'll go back and see what on the respiratory side might be causing things.
Luke Lemons (07:49):
Exactly. So they come in irritated of having an itchy mouth. And especially when it comes to peanuts and tree nuts, that is something that parents get really nervous about. And so they wanted to take their children in to be evaluated. And so as a clinician, you think, okay, first is it a peanut allergy? Is it a treated
Gary Falcetano (08:08):
Allergy? The history seems consistent with that, where you have symptoms on ingestion, close proximity to the ingestion. So the next step would be a specific IgE test for peanut. And the best, most efficient way to do that is with peanut, with reflex to the peanut allergen components. And we'll talk through that in a minute. But that way, only one blood draw. If the whole extract is positive, then it will reflex and give us an idea of what in that peanut is actually driving symptoms.
Luke Lemons (08:36):
And then the same for Trina. There's Trina allergen components as well. And so let's say they come back with levels of peanut IgE that they aren't alarming.
Gary Falcetano (08:48):
Now sometimes they might even be, but yeah, they're certainly positive. They're certainly elevated levels. Without going any further, a number of clinicians may just make the diagnosis of peanut allergy. We have symptoms, we have a positive test, we correlate the two. That's peanut allergy. But because she didn't have severe or systemic symptoms, and also because we know she has some seasonal allergy symptoms, it's really good idea to look at those components. And when we look at those components, they can tell us a lot. So maybe do you want to,
Luke Lemons (09:17):
Yeah. So again, after we understand that it potentially could be a food or a peanut allergy, well, there's all the evidence there to diagnose history and results. Have they been experiencing respiratory symptoms, especially during the springtime and maybe the summertime, and looking at their respiratory triggers as well and seeing what might be causing that kind of reaction? Because if it comes back as, what is it? Birch pollen, correct?
Gary Falcetano (09:43):
Yeah. So birch pollen is highly correlated, right? With the food pollen allergy syndrome for peanut. And that typically would be driven by one of those peanut components, RH eight, it's a BET V one protein. It's a homologous protein with birch pollen. So if we look at the component profile first, in this case, we would've seen that she was only positive for the RH eight, the BET V one protein, meaning that it's being driven by the pollen sensitization, and if she's negative for those storage proteins. And those of you that we can refer you back to that episode on the peanuts and tree nuts where we go into detail on the peanut components, but the storage proteins are more correlated with systemic allergy. And she doesn't have any of that positivity here.
Luke Lemons (10:29):
And all this to say, the reason we're having this conversation is being that it's springtime. There may be elevated cases of patients coming in who have itchy mouth and parents who are saying, my child has this food allergy. They're allergic to apples, they're allergic to tri nuts. They're allergic to peanut
Gary Falcetano (10:45):
100%.
Luke Lemons (10:46):
And we have to be very careful during this time because there are cases in which patients do have a true severe peanut allergy coming in and saying the same thing. So we need to differentiate pollen food allergy syndrome from food allergy this spring, and really any of these big pollen to a more
Gary Falcetano (11:01):
Severe form of food allergy. Right,
Luke Lemons (11:03):
Exactly.
Gary Falcetano (11:03):
Yeah. So I think when someone presents, we address the food allergy with the peanut and the components, now we see that it's probably the birch pollen driving these symptoms right now. The risk is lower now on the food side, but we really didn't address the respiratory symptoms, and we should do that too, right? Looking at the whole person. She's got symptoms in the spring and fall. Let's see, what exactly in the respiratory side of things is driving those symptoms? It probably isn't just the tree pollen.
Luke Lemons (11:30):
Oh yeah. What is it? 90% of patients are polys sensitized.
Gary Falcetano (11:34):
Yeah. Up to 90% of patients who are allergic more than one thing. So yeah, that's probably the tree pollen for sure, because we see the protein that's homologous with tree pollen in the peanut. But what else? So we may see that it's birch tree, we may see that it's a dog. We may see that it's dust mite. And remembering, going back to our cumulative threshold episodes, allergens are additive. So identifying all of the allergens that they're sensitized to that may be driving symptoms can really help them from a preventative medicine standpoint to address those, bring down their symptoms. And PS, sometimes those pollen food allergy symptoms are worse in the spring because of that same cumulative threshold. They're having tree pollen, plus they're ingesting a peanut that looks like tree pollen and boom, you've got
Luke Lemons (12:21):
Some. So if a patient has elevated levels of let's say dog dander and then birch pollen, and they're sneezing, if we lower the levels of dog dander, they might not be sneezing anymore. And also, they might not have the tingling in their mouth when they eat a peanut.
Gary Falcetano (12:36):
It's very, very possible. And again, this is preventative medicine, right? It's actually looking at what's causing symptoms and decreasing exposure. Remember we talk about you don't have to put people in a bubble. Even when it comes to the tree poll, there's ways of decreasing exposure, especially in the bedroom where we spend 8, 9, 10 hours a day making sure that pollen doesn't get in the bedroom. If it's the pet, making sure the pet stays out of the bedroom, it's the dust mite, putting the covers, washing the sheets. So all those things to protect that sleep space can improve their respiratory symptoms and potentially improve their pollen food allergy syndrome.
Luke Lemons (13:07):
Yeah. Yeah. It's really pollen food allergy syndrome. This spring should be taken as an opportunity to really evaluate your patients.
Gary Falcetano (13:15):
You're getting excited
Luke Lemons (13:16):
Here. Yeah, no, because I think it's really interesting. We always talk about, Gary and I talk about allergies all the time, and it's always respiratory allergy, food allergy, and this is that bridge that really brings it full circle. So why don't we get into some management strategies when it comes to avoidance.
Gary Falcetano (13:32):
So I think we already talked about decreasing exposure to the pollens, but then when we're talking about the foods themselves, for instance, apples.
Gary Falcetano (13:40):
So there is people that can ingest apple pie, eat apple pie, and have no symptoms. Going back to how these proteins get denatured, the high heat of the baking process denatures those food pollen allergy proteins, that causes a reaction. But when they eat a regular apple, they may have symptoms. So baking foods, there's certain other proteins like the lipid transfer proteins that are concentrated in the skins of fruits. So in that case, just peeling the fruit may actually help with that. These all need to be individualized because remember, it is a spectrum of symptoms and we do have to be careful always the potential for severe allergy. And I think that brings us to also, there needs to be individual decision-making around prescribing an epinephrine autoinjector. Or now we have inhaled epinephrine as well, but some type of emergency rescue epinephrine, there needs to be a discussion. Is the patient at higher risk where that's indicated? Are they at low risk where you maybe discuss how does the patient feel about that?
Luke Lemons (14:42):
And again, components can help with those conversations as well and understand.
Gary Falcetano (14:46):
And for a lot of the allergens,
Luke Lemons (14:47):
Certainly. Yeah. And so we mentioned with peanut, it was RH eight. Let's say that I'm a provider and I got tree nut allergy components for a patient who has an itchy mouth from eating.
Gary Falcetano (14:57):
So for instance, with hazelnut, there actually is a protein that's homologous with birch pollen, and that's Cory one. The CO one protein is just like the RH eight in the peanut. It's Cory one in the hazelnut.
Luke Lemons (15:10):
So a patient that if I get the results back and it's CO A one, we might be looking at pollen food allergy syndrome.
Gary Falcetano (15:17):
Exactly. Just like when it was co. And then there's other components like prophy flynns. The prophy flynns are the same in tree nuts. And the peanut, they're responsible often for the food pollen allergy syndrome, and they are found in pollens tree pollens. So they're pretty ubiquitous in all the plant pollens.
Luke Lemons (15:34):
Okay. We do have, for anybody who's listening out there, we do have interpretation guides for peanut and Trina Aller components, the outlines, we talk about profil on there. We talk about these specific components associated with pollen food allergy syndrome. So in the description of this episode, there'll be a link if that's interesting to you, if
Gary Falcetano (15:51):
You want. Exactly. And they also discuss those kind of species specific storage proteins that are more high risk that would lead to this not being the food pollen allergy syndrome, but more a systemic, potentially severe food allergy.
Luke Lemons (16:05):
And again, this is all to say that this is happening during the springtime. And so we really wanted to just make this episode to highlight the other half of spring, which is oddly food. We always used to say, well, we always still do say you can't control the pollen, but in this case, the pollen could be an indicator for so much more. Yeah, exactly. So if you have patients who are coming in the spring with itchy mouth, of course, if it's from peanut, Trina, other foods, let's evaluate them for food allergy. Let's be sure. And then looking at their respiratory triggers, are they suffering from rhinitis during this time? Have they been evaluated? It's again, a great opportunity for a full allergy understanding of a patient
Gary Falcetano (16:48):
100%. And how can we use kind of preventative medicine techniques to reduce their exposure on the respiratory side better understand their symptoms on the food side, and really just generally improve their quality of life with this kind of pollen apocalypse that we're in for right now.
Luke Lemons (17:04):
Well, thank you everyone for listening. Again, the link in the episode's description will take you to a page that will have interpretation guides for peanut and Trina, as well as a lab ordering guide, which has some respiratory profiles that are location specific from the labs that you probably already use. Thank you for listening to cast and have a good spring.
Gary Falcetano (17:23):
Yeah, we'll see you next time. Thanks. Thanks.
Announcer:
ImmunoCAST is brought to you by ImmunoCAP Specific IgE Testing and Phadia Laboratory Systems, products of Thermo Fisher Scientific. For more information on allergies and Specific IgE Testing, please visit Thermofisher.com/ImmunoCAST. Specific IgE Testing is an aid to healthcare providers in the diagnosis of allergy and cannot alone diagnose a clinical allergy. Clinical history alongside Specific IgE Testing is needed to diagnose a clinical allergy.
The content of this podcast is not intended to be and should not be interpreted as or substitute professional medical advice, diagnosis, or treatment. Any medical questions pertaining to one's own health should be discussed with a healthcare provider.
- Carlson G, Coop C. Pollen food allergy syndrome (PFAS): A review of current available literature. Ann Allergy Asthma Immunol. 2019 Oct;123(4):359-365.
- Ciprandi G, Alesina R, Ariano R, et al. Characteristics of patients with allergic polysensitization; the polismail study. Eur Ann Allergy Clin Immunol. 2008;40 (3);77-83.

Legal manufacturer: Phadia AB.
Before you proceed ...
We noticed you may be visiting a version of our website that doesn’t match your current location. Would you like to view content based on your region?
Talk with us
Interested in utilizing our solutions in your laboratory or healthcare practice?
This form is dedicated to healthcare and laboratory professionals who work within medical laboratories, private practices, health systems, and the like.
By clicking "continue with form" you are confirming that you work within a healthcare or laboratory space.
Not a lab professional or clinician but interested in diagnostic testing for allergies?
Visit Allergy InsiderChoose your preferred language
Please note: By selecting a different language, you are choosing to view another site. Product availability and indications may vary from what is approved in your region.