Episode 028
Preparing Asthma Patients for Spring: Strategies and Insights
-
Summary
-
Episode Resources
-
Transcript
-
Related Episodes
Episode summary
Coming out of the winter months and flu season, we dive into the best ways to help prepare patients with asthma for the spring allergy season. From insights into the impact of allergies and viral illnesses on patients with asthma to ways to help reduce exposure to potential allergic triggers, tune in and gain important information on how you can help optimize patient outcomes going into spring.
Episode resources
Find the resources mentioned in this episode
Lab Ordering Guide
Looking for allergy diagnostic codes from the labs you already use?
Episode transcript
Time stamps
0:41 - Current Flu and Pollen Data
1:43 - Asthma Triggers and Unified Airway Concept
2:52 - Asthma, Viral Illness, and Allergy Risks
4:31 - Preparing Asthma Patients for Spring
5:57 - Polysensitization and Personalized Approach
7:15 - Stepwise Approach to Asthma Management
10:08 - Specific Allergen Reduction Strategies
14:21 - Inner City Asthma Study Findings
15:58 - Preparing for Spring Allergy Season
17:19 - Resources and Conclusion
Announcer:
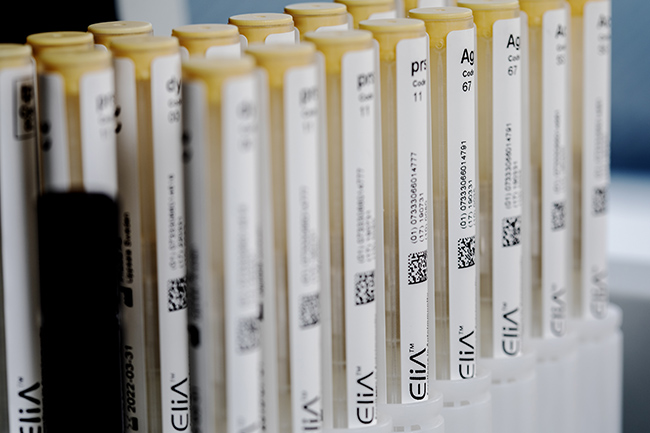
ImmunoCAST is brought to you by ImmunoCAPTM Specific IgE testing and PhadiaTM Laboratory Systems, products of Thermo Fisher Scientific. The content of this podcast is not intended to be and should not be interpreted as a substitute for professional medical advice, diagnosis, or treatment. For patients any medical questions pertaining to one's own health should be discussed with a healthcare provider.
Gary Falcetano: I'm Gary Falcetano, a licensed and board certified PA with over 12 years experience in allergy and immunology.
Luke Lemons: And I'm Luke lemons, with over 6 years experience writing for healthcare providers and educating on allergies. You're listening to ImmunoCast, your source for medically and scientifically backed allergy insights. Welcome to ImmunoCast. We have a timely and important episode lined up today around asthma and allergies coming out of the winter. And considering the flu season that's happening right now.
Gary Falcetano: Yeah, you know, we were looking at some CDC data around influenza prevalence, and also we're seeing a lot of activity in the news around early pollen seasons. You know, not only here in Florida, where I live, but as far north as Atlanta.
Luke Lemons: Already looking at that CDC data, Gary and I saw, you know, there's almost an 8% increase in visits to healthcare providers this week for respiratory illness this week. And just to mind you, we're recording on February 10th.
Gary Falcetano: Yeah. And at the same time, we're seeing items in the news where Atlanta has hit high pollen levels at the earliest time, I think pretty much ever recorded.
Luke Lemons: Oh, wow.
Gary Falcetano: This early in the season. Yeah, the first week of February.
Luke Lemons: Considering all of this, we figured that we wanted to make an episode for you guys today around preparing those patients who do have asthma for the incoming spring pollen season. Being that we're coming out of this cold winter, the flu is now a factor, and we want to make sure that these asthma patients have some sort of relief for the first half of this year.
Gary Falcetano: Exactly. Because we know when we're talking about asthma, Right. Especially allergic asthma, but really any type of asthma, we're talking about airway inflammation and all of those things that kind of can trigger increased inflammation in the airways, whether they be allergies, whether they be viral illnesses, whether they be weather changes, cold air, increased humidity, all of these things can kind of snowball. Right. And that's why in the fall, we talk about asthma peak week as being so significant. We're seeing that again now this late winter where we have flu season really colliding with spring pollen season.
Luke Lemons: And this has to do with the unified airway you had mentioned, weather, the flu, the cold, I mean, all that affects the same airway, which is why we get these exacerbations.
Gary Falcetano: Yeah, exactly. We know that, you know, what affects one portion of the airway often triggers Responses in another part of the airway. Right. We know that, you know, the unified airway concept is that it is one airway from the tip of the nose till the alveoli. Right. And often what causes reactions like rhinitis in the nose can trigger worsening of symptoms with. Especially with someone with allergic rhino or allergic asthma.
Luke Lemons: So going back to the flu really quick, before we go into some preventative actions that you can take with your patients, it's really interesting to note that a patient with asthma and a viral illness is three times more at risk of being hospitalized than someone without asthma. And so that's a big number.
Gary Falcetano: Yeah, and that makes sense. Right, because they're both kind of triggers for that airway inflammation. So, you know, both of them together are really, you know, quite cumulative.
Luke Lemons: What's even more shocking is that if a patient with asthma has a viral illness and is exposed to an allergen that they're also sensitized to, that risk factor jumps to 20 times.
Gary Falcetano: So what you're saying is the risk of being hospitalized. And I think this study was by Murray and colleagues. Right. And this was looking at children and visits to emergency departments. But, yeah, if you have kind of that triple whammy, Right, being exposed to a viral illness or having a viral illness, being allergic and then being exposed to those triggers, that triple whammy increased their chances of being hospitalized by 20 times.
Luke Lemons: Yeah. And I mean, even just looking at the numbers from viral illness and asthma, which is three times, and then just adding the allergen element jumps to 20 times. And we know that allergies drive asthma symptoms in both adults and children.
Gary Falcetano: The numbers are, you know, as much as 60% of adults with asthma and 90% of children with asthma actually have allergies that play into their asthma symptoms.
Luke Lemons: And this is partly why the CDC has guidelines that say that patients with persistent asthma need to be evaluated for potential allergic triggers. And this is also why the NIH says it's Category A evidence that they be evaluated for their allergic triggers.
Gary Falcetano: Yeah, we've talked about this before, Luke, but I don't think, you know, there's anybody out there that wouldn't consider at least offering an influenza vaccine to their patients with asthma. And actually, in the NIH guidelines, there's only category B evidence. So there's actually more evidence being Category A for assessing allergic triggers than there is for the influenza vaccine. So, you know, it kind of goes without saying we need to assess these allergic triggers in every patient with persistent asthma.
Luke Lemons: So knowing these risks and how the asthma and allergies kind of interrelate with one another. What can we do to set up patients who have asthma for success going into the spring? Being that they may have had a.
Gary Falcetano: Rough season so far, I think certainly we need to be sure. You know, we mentioned this as well in previous episodes. We know that, you know, asthma patients sometimes when they're. When they're feeling okay. Okay. Tend to stop utilizing their controller medications. That it's important that, number one, they have prescriptions for the appropriate controller medications. Number two, they're using them appropriately, especially if they have been kind of avoiding the flu. Feeling a little bit, you know, feeling pretty good right now. And we're expecting, you know, a pretty bad allergy season coming. We want to make sure that they're, you know, continuing to take their controller medications appropriately. But then, of course, with allergy season coming up, knowing what they're potentially sensitized to can really help them to do kind of a more preventative medicine approach to really help reduce their exposure to those sensitized triggers.
Luke Lemons: And I think oftentimes we think, oh, well, it's pollen. Like, what can we do about pollen? I have patients who have allergic asthma. They're probably allergic to the tree pollen. It's really just making sure they have enough of their medicine. But really, 80% of people who do have allergies are polysensitized. So there's probably something else that may be contributing to your patients with allergic asthma symptoms.
Gary Falcetano: Exactly. And, you know, we're not just, you know, typically, we're not just talking about two different types of tree pollen sensitizations. Right. We're talking about sensitizations that can really be across the board and especially include some of those perennial or indoor allergens. So the ones that aren't as easily identified just by saying, oh, it's spring, you know, tree pollen season. It must be tree pollen allergy. By actually looking at objective evidence of what they're sensitized to, we can figure out, is it dust mite, Is it the pets, Is it mold along with that tree pollen? Or maybe even, you know, not including that tree pollen. But we get a more personalized kind of snapshot of exactly what's going on with the patient.
Luke Lemons: Yeah. And when we see that snapshot that this is where you had spoken about it briefly before, but making sure that with their medicine and their medication that they have enough, but then also evaluating these patients to maybe step down on some medication. So that the stepwise approach. Right.
Gary Falcetano: Yeah. I mean, you know, I think. I think most providers that treat asthma, are familiar with the NIH guidelines, at least, have seen that stepwise approach to treating asthma in most drug references. Right. In most online references. Typically, we keep escalating dosages of medications, adding in additional medications to get patients under control. But I think, you know, it's important that we remember that those steps can go down as well as up. Right. So if we are able to identify some triggers that are actually driving their symptoms, reduce exposure to those triggers. Right. They may not need as much in the way of multiple medications or dose dosages of medications to keep them really in a controlled state. So, you know, remembering, we can go up and down. It's not just an up escalator, but it's an up and down. Right. That we can follow.
Luke Lemons: And it's a balance. Going into this spring allergy season, we're saying that making sure that they have medication doesn't mean the recommendation is just to up the medication to prepare them. No. Right, Gary. It's a balance of trying to understand what are causing symptoms so that we can reduce that while also making sure that they have the appropriate medication at the same time getting that medication under control.
Gary Falcetano: That's absolutely correct, Luke. And I think, you know, we tend to not always think about all of the potential side effects from medications. Right. And these medications are amazing, but really our ultimate goal is to have them on the lowest effective dose to minimize any potential side effects, things like adrenal suppression or localized issues with even inhaled, you know, nasal steroids. So, yeah, I think really looking at
the whole patient and finding out those things that really are very low cost or no cost that they can do. Right. To reduce their symptoms and actually make the medications more efficacious.
Luke Lemons: I'm glad you bring up cost, because that's just another thing that I think we need to consider is a lot of these medications aren't cheap, and we can help the patient from an economic point of view as well by giving them an option to breathe easier by reducing exposure to potential triggers. Recently there was in the news, I believe, there's a man who had to stop taking his medication due to a price hike and ended up, unfortunately, dying. It's a real stress on patients, the cost of medication. And so we want to make sure that we're giving them options that they can go home and do for low. Low costs.
Gary Falcetano: Exactly. You know, potentially. Right. If we can get their exposures reduced to those allergy triggers, being on a lower dose medicine or not being on a more costly combination medicine can really have an effect. Not Only, you know, on their health, but on their pocketbook.
Luke Lemons: So let's maybe go over a few examples on how to reduce exposure for some specific allergens. So let's say that you have a patient with allergic ASTH and you evaluate them for their allergic triggers and they come back, let's say with elevated levels to tree pollen, but then also let's say cockroaches. What can we do there to help these patients?
Gary Falcetano: Yeah. So first I think, you know, I want to call out, right. That we have resources to help providers to help patients. Right. So patient education materials, targeted exposure reduction sheets that make this education really straightforward for providers. Make it very quick, it doesn't take a whole lot of time. But where, once we've identified their allergic trigger triggers, we can tell them what is recommended. Right. To reduce their exposure and, you know, through shared decision making, kind of get their buy in on what's possible. So I think, you know, what you said, Luke, what's something you can do for. If we have a identified pet allergy?
Luke Lemons: Keeping the pet out of the bedroom is a big one. I know that's really hard. It's a hard conversation for some patients who just love sleeping with their dog or cat. But keeping them out of the bedroom, making sure the clothes that they're wearing, if they are playing with their, their pet don't, you know, go into the bedroom as well. Being that we spend a majority of our time they're sleeping and breathing, I think those are some starting points for pets.
Gary Falcetano: Yeah. And I think, you know, so you kept mentioning bedroom and I think, you know, the term we've used before is a safe sleep space.
Luke Lemons: Yes.
Gary Falcetano: Right. Not putting patients in a bubble. But if allergens are found somewhere outside of the bedroom, whether that be pets or pollens, do whatever we can to keep those allergens from getting in the bedroom. So if it's pollens keeping the windows closed, you mentioned, you know, changing clothes. Right. If you're outside working or playing in high pollen season, you want to change those clothes before you bring into the bedroom, before you go to, you know, should never sleep in those same clothes you've been outside with. For sure. You know, washing your hair if there's pollen will be attracted to your hair. I mean, you know, both Luke and I are a little follicly challenged. That's not an issue for us, but it certainly is. You, you know, you put that whole head full of hair full of pollen into your pillow and, and sleep with it. So there's, you know, there's a lot of things that we can do, you know, around dust mites and we've talked about that and controlling humidity levels, et cetera.
Luke Lemons: And I think with the dust mites especially too, we say all these things and sometimes there may be some doubt to be like how impactful is it actually to keep a safe sleep space for patients. And there's actually been research into the impact of these kind of low cost reduction of exposure methods.
Gary Falcetano: Yeah. You know, specifically around dust mites there was a great study by Halkin and colleagues that actually looked at just dust mite allergen covers. So you know, that was the only variable in this study was the active group that were dust mite sensitized. So they had dust mite allergy, used these dust mite covers. What were some of the findings after a year of using these covers in these kids who were all had asthma. Right. And they were all on inhaled corticosteroids.
Luke Lemons: Yeah. So all of them had asthma and were on that medication. And by just changing to dust mite covers we saw a 50% reduction in inhaled steroid use.
Gary Falcetano: So that's amazing to me. Right. Because a one time purchase and you know, we know we can get these covers at discount stores like you, you don't have to be at a, at some high end store to get these dust mite allergen covers. That's all they did. They didn't do even some of the other recommendations around reducing dust mite concentrations like make keeping humidity between 30 and 50% et cetera. They just used the dust mite covers and they saw a 50% reduction in inhaled corticosteroid use. Think of what that translates to. Number overall, you know, they're very safe drugs, but overall decrease in amounts of steroids, even topical that patients are, you know, were exposed to. But also from an economic standpoint. Right. A 50% reduction in medication use.
Luke Lemons: We say all this again going into spring allergy season where a lot of patients who do have allergic asthma can't control the amount of pollen that's in their air. And you had mentioned a few states, Gary, where pollen season is already happening right now. But, but by knowing and knowing his power, by knowing what else may be contributing to symptoms, there's things that we can do actively in front of us that can help these patients breathe easier. So again, the dust mite cover one is huge. And this isn't an ad for dust mite cover, by no means, but it just kind of proves that taking action at home, outside of just, just medication use does Impact patients.
Gary Falcetano: Exactly. And we've seen other studies and we've talked about that. The Morgan inner city asthma study that talked about bedroom only interventions, not just dust mite. Right.
Luke Lemons: Why don't we talk about that just really quickly? Do you mind just skipping over that?
Gary Falcetano: No, sure, sure. So, you know, for those of you that hadn't heard this in previous episodes, the Morgan study was published in the New England Journal of Medicine. It had about a thousand participants, inner city children from all over the country, Boston, New York, Atlanta, Phoenix, and basically randomized two groups. Both groups got excellent care, guideline based care, optimized their medications, their education. The only difference between the two groups, the active arm, was evaluated for their allergic triggers. They had testing and they did bedroom only interventions to reduce their exposure. And what they found was a pretty dramatic reduction in multiple measures. So I'm trying to remember because I don't have any notes in front of me, Luke, but I believe it was three weeks less symptoms per year in the active arm. It was almost a week's less missed school. I think it was four point some days less missed school days per year, and I think about two less unscheduled office arrear visits. Again, all from just identifying their allergic triggers and reducing them in the bedroom.
Luke Lemons: So again, we say all this because looking forward into spring, if you do have patients who have asthma, now is the time to flag them when they come in and make sure that they're prepared. Have they been evaluated for their allergic triggers per CDC and NIH guidelines? Are they up to date on their medication? Is there any opportunity to reduce exposure to potential allergens at home?
Gary Falcetano: I would add, we didn't really talk about this, but for those patients that have allergic asthma that have rhinitis symptoms, we know there's this concept of priming, right, where if we start getting exposed to our allergens and we start treating them after the fact, they're a lot harder to control with medications. So it's important too, when we know that someone is allergic to tree pollen, say, and we know tree pollen season is going to start in the next two weeks, that maybe they start with their inhaled nasal steroids. Right. To prevent that priming kind of concept from making it even harder to control those symptoms, that combined with educating them on proper exposure reduction techniques can all kind of combine to really make this spring pollen season a lot better for our patients with asthma.
Luke Lemons: Yeah, and I'm glad you mentioned the priming too, because it's not just the pollen that can prime too. If they have let's say a bad pet dander allergy like that, that going in can also, with the pollen combined, elevate these levels. So it's really making sure that they're prepared in all facets of allergens going in 100%.
Gary Falcetano: So if we can start reducing those exposures to the pets before spring pollen comes. Right. If we have that cumulative threshold kind of concept where the pet allergen and inflammation from being exposed to those is adding onto the pollen inflammation, let's start reducing everything that we can to, again, make this, you know, much less symptomatic season.
Luke Lemons: Exactly. And we do have on this episode's webpage some resources and there's a link in the description of this episode to that webpage. We have resources around, you know, ways that we can reduce exposure to specific allergens. So, you know, target exposure reduction plans, which speak to different ways that we can reduce exposure to specific allergens, as well as a lab ordering guide which has codes for profiles, respiratory profiles for region specific allergens that may be affecting your patients. So if you do have patients
with asthma coming in and they haven't been evaluated, this is a good resource for the labs that you most likely already use.
Gary Falcetano: Yeah, and we'll put some additional resources there as well, like interpretation guides. So everything will be kind of in one place to really be able to make it easy to help our patients this time of year.
Luke Lemons: So thank you again for listening to this episode around asthma and allergy. And let's be sure that patients going into the spring are breathing as easy as they can by looking at some of their allergic triggers. And we hope that you enjoyed this episode.
Gary Falcetano: Yeah, absolutely. Thanks so much and we'll see you next time.
Immunocast is brought to you by Thermo Fisher, scientific creators of immunocap specific IgE diagnostics and Fadia Laboratory Systems. For more information on allergies and specific IGE testing, Please visit thermo fisher.com immunocaf Specific IGE testing is an aid to healthcare providers in the diagnosis of allergy and cannot alone diagnose a clinical allergy. Clinical history alongside specific IgE testing is needed to diagnose a clinical allergy. The content of this podcast is not intended to be and should not be interpreted as, or substitute professional medical advice, diagnosis or treatment. Any medical questions pertaining to one's own health should be discussed with a healthcare.
- “FluView.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, www.cdc.gov/fluview/index.html. Accessed 17 Feb. 2025.
- Murray CS, Poletti G, Kebadze T, Morris J, Woodcock A, Johnston SL, Custovic A. Study of modifiable risk factors for asthma exacerbations: virus infection and allergen exposure increase the risk of asthma hospital admissions in children. Thorax. 2006 May;61(5):376-82.
- Allen-Ramney F, Schoenwetter W, Weiss T, et al. Sensitization to Common Allergens in Adults with Asthma. JABFP. 2005;(18)5 434-439.
- Host A, Halken S. Practical aspects of allergy-testing. Paediatr Respir Rev. 2003; (4) 312-318.
- National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007 Nov;120(5 Suppl):S94-138
- Asthma fact sheet - centers for disease control and prevention [Internet]. [cited 2024Feb5]. Available from: https://www.cdc.gov/asthma/pdfs/aa_fact_sheet.pdf
- Ciprandi G, Alesina R, Ariano R, et al. Characteristics of patients with allergic polysensitization; the polismail study. Eur Ann Allergy Clin Immunol. 2008;40 (3);77-83.
- Halken S, Høst A, Niklassen U, Hansen LG, Nielsen F, Pedersen S, Osterballe O, Veggerby C, Poulsen LK. Effect of mattress and pillow encasings on children with asthma and house dust mite allergy. J Allergy Clin Immunol. 2003 Jan;111(1):169-76.
- Morgan WJ, Crain EF, Gruchalla RS, O'Connor GT, Kattan M, Evans R 3rd, Stout J, Malindzak G, Smartt E, Plaut M, Walter M, Vaughn B, Mitchell H; Inner-City Asthma Study Group. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004 Sep 9;351(11):1068-80.

Legal manufacturer: Phadia AB.
Before you proceed ...
We noticed you may be visiting a version of our website that doesn’t match your current location. Would you like to view content based on your region?
Talk with us
Interested in utilizing our solutions in your laboratory or healthcare practice?
This form is dedicated to healthcare and laboratory professionals who work within medical laboratories, private practices, health systems, and the like.
By clicking "continue with form" you are confirming that you work within a healthcare or laboratory space.
Not a lab professional or clinician but interested in diagnostic testing for allergies?
Visit Allergy InsiderChoose your preferred language
Please note: By selecting a different language, you are choosing to view another site. Product availability and indications may vary from what is approved in your region.