Episode 031
Understanding the Allergy Symptom Threshold with Dr. Zachary Rubin and Allergy Insider
-
Summary
-
Episode Resources
-
Transcript
-
Related Episodes
Episode summary
In this episode of ImmunoCAST, we share an example of impactful patient education from our friends at Allergy Insider (@allergyinsider). They hosted Dr. Zachary Rubin (@rubin_allergy), a double board-certified pediatrician and allergist and internet sensation, and ImmunoCAST’s own Gary Falcetano, PA, on their recent Instagram Live segment “Ask the Insider” to discuss the allergy symptom threshold.
Because Allergy Insider aims to provide patients with evidence-based, educational information about their allergic conditions, helping them feel more empowered and informed about their health, Allergy Insider is a perfect source to refer your patients to if they want to learn more about their allergic conditions. Tune in and discover some helpful tips you can share with your patients when discussing reducing exposure to their allergic triggers.
Guest spotlight

Dr. Zachary Rubin
Zachary Rubin, MD, FACAAI, is a double board-certified pediatrician specializing in allergy treatment and immunology. He has gained a following of millions of users across TikTok and Instagram, creating educational allergy-related content for patients and clinicians alike.
Episode resources
Find the resources mentioned in this episode
Lab Ordering Guide
Looking for allergy diagnostic codes from the labs you already use?
Episode transcript
Time stamps
2:12: Dr. Zachary Rubin introduced on Ask the Insider
3:48: Explaining the allergy symptom threshold concept
5:56: Oral allergy syndrome and food allergies
7:30: Importance of allergy testing and triggers
9:58: Strategies to reduce indoor allergens
12:22: Humidity, dust mites, and bedroom allergens
14:00: Seasonal pollen patterns across regions
16:12: Medication timing and allergy "priming"
18:01: Why allergies change over time
Announcer:
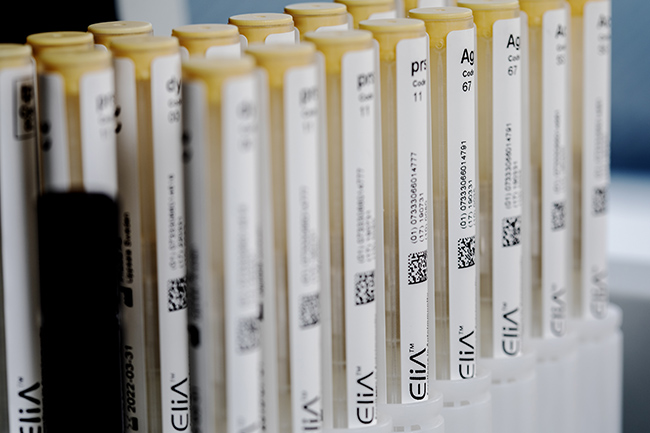
ImmunoCAST is brought to you by Thermo Fisher Scientific, creators of ImmunoCAP™ Specific IgE diagnostics and Phadia™ Laboratory Systems.
Gary Falcetano:
I'm Gary Falcetano, a licensed and board-certified PA with over 12 years experience in allergy and immunology.
Luke Lemons:
And I'm Luke Lemons, with over six years experience writing for healthcare providers and educating on allergies. You're listening to ImmunoCAST, your source for medically and scientifically-backed allergy insights.
Welcome to ImmunoCAST. As many clinicians know, patient education is an extremely valuable tool when it comes to helping a patient not only understand their condition, but also to ensure that they have credible and factual information. That's why in this episode, we're going to share a patient education conversation that happened between Gary Falcetano and Dr. Zachary Rubin. This conversation took place on Allergy Insider's Instagram.
And if you're not familiar with Allergy Insider, they're our friends who are more patient-facing. They have conversations that are more accessible to patients around allergies. They have a website, but they also have an Instagram page. And on this Instagram page, they'll go live with an expert and talk through some topic related to allergies for patients who are interested in learning.
We've had Dr. Rubin before on ImmunoCAST. That was in episode 24 where he discusses navigating social media as a clinician. And it's a great episode, I recommend checking it out. This episode specifically is a recording of an Ask the Insider Live. So on Allergy Insider, they went live with Dr. Rubin, and Gary serves as host who discusses the symptom threshold of allergies, which is the idea the allergies actually stack and it may not be one trigger that is contributing to these symptoms. It's a great conversation and it's also a great example of the type of patient-facing education our friends Allergy Insider provide.
So enjoy this episode and don't forget to check Allergy Insider out on Instagram, as well on their homepage, which will be linked in the episode page in the description below.
Gary Falcetano:
I want to welcome everyone to this episode of Ask the Insider. This is Inside Spring Allergies, totally appropriate for first day of spring, and we're going to be discussing the allergy symptom threshold. I'm Gary Falcetano, your host. I've been a PA for over 28 years, currently the US Scientific Affairs Manager for Allergy at Thermo Fisher Scientific.
Joining me today is my special guest, Dr. Zachary Rubin. He's a double board certified allergist, a bit of an internet sensation with millions of followers on Insta and TikTok. We're going to dive deep, as we were saying, into the concept of the allergy symptom threshold and how understanding it can help manage allergic reactions a little bit more effectively. So welcome, Dr. Rubin.
Zachary Rubin:
Thank you so much for having me. And I've had some chats with you before, it's been fun getting to know each other and talk about what I'm really passionate about. And this is one topic that I actually haven't talked about in a while, so I think a lot of the people here are going to learn something new today.
Gary Falcetano:
Yeah, absolutely. I'm so happy to have you. And as you were saying, it's been great at our past experiences. And this is one of my passions as well. I love talking about allergy, I love talking about how we can really empower patients to really take control of their disease and better manage their symptoms.
So you know what? Let's start out with the basics today. So it is the first day of spring. Spring allergies, tree pollen are already major issues in many parts of the country. Although in Chicago, I understand it's snowing today, so maybe you've got a few day reprieve. Maybe discuss this concept of allergy symptom threshold and why it's so important and why it may not just be tree pollen that's driving symptoms this time of year.
Zachary Rubin:
Exactly. So when you develop allergies to pretty much any substance, your immune system has this abnormal response that will generate different substances. The ones that we normally think of are called a Type I hypersensitivity reaction. So you make these antibodies, these proteins called immunoglobulin E, or IgE for short. So if you develop an allergy to tree pollen to dogs, food, et cetera, if you are exposed to that, there's a certain threshold, we were calling it the symptom threshold, where you need to have a certain amount of exposure before the symptoms develop.
So think of it like you have a cup and you fill it with either water or marbles. So if you're allergic to multiple issues and you get exposed to all of them at the same time, you're filling that cup up until you reach that threshold. And once you start having more exposure, it spills over and leads to symptoms.
Now, that threshold can change over time and it can have different situations where, let's say you have a viral illness, that could potentially lower your threshold. You have a fever, that could lower your threshold and increase the risk of having more severe symptoms. Same thing with exercise or consuming alcohol, these different issues can lower the threshold before you start to have symptoms.
And it's not always these specific allergic triggers, they could be non-allergic in nature like just the sheer fact that we're having change in weather. Where I'm at right now, we had a big thunderstorm yesterday, the temperature was in the 50s, and it's dropped to below freezing and now we have a snowstorm and there's about one to two inches of snow on the ground on the first day of spring. So that change in temperature, in barometric pressure can also fill up the cup, so to speak, and lead to symptoms getting worse.
Gary Falcetano:
Exactly. And it's not just rhinitis or upper airway symptoms that are so common in the spring, but this also leads into other even lower respiratory symptoms like asthma. We know that a large majority of patients with asthma have allergic triggers. And those that don't even sometimes have non-allergic triggers that contribute through that inflammation, right?
Zachary Rubin:
Right, exactly. There's so many different ways that our immune system interacts with our environment. And food as an example, there's something called oral allergy syndrome where you have this allergy to pollen from birch tree is the classic example because it's got protein structures similar to peaches, pears, plums, apricots, all these different fresh fruits that when you eat it, your immune system gets confused and thinks, "Oh my gosh, I think I'm eating a bunch of pollen." And if you do that, especially in pollen season, that threshold is going to get filled up very quickly and you're going to develop itchy mouth, mild swelling, and in rare cases can become more systemic and lead to anaphylaxis.
And this is true with food allergies as well, where a small amount for some people may not hit that threshold before having symptoms. Maybe it's a couple milligrams of protein before you start having symptoms. But if you're sick, lowers that threshold, increased risk of having hives, swelling, problems breathing. It's all sorts of other symptoms that are not necessarily related to your nose.
Gary Falcetano:
Absolutely. And these thresholds, as you mentioned, they change. They can differ at different times of the year for patients, again, depending on what a patient is experiencing, like a viral illness. But we also see patients who are experiencing symptoms this time of year. I think our fallback is to say, "Well," especially in areas where we know tree pollen is prevalent, "it must be the tree pollen." But what can we do, and I'm thinking about testing here, to actually understand all of the things someone may be sensitized to on the allergic side, right? Non-allergic is a little more history dependent.
Zachary Rubin:
Exactly. So when I evaluate a patient and thinking about, okay, what are the potential triggers for their symptoms of rhinitis, we do a full panel of environmental testing. So that test, whether it's skin or blood testing, can give us a good idea of what amount of allergy antibody is present that could bind to that particular substance and lead to symptoms. And then you can look at the history correlated to the testing to determine, okay, I find that actually you're not only having symptoms to tree pollen but mold. And when it gets very humid outside or maybe there's water damage in the home, they're getting exposed to mold on top of the pollen exposure. So those multiple exposures can lead to symptoms.
So if we do targeted environmental reduction strategies, like saying, "Okay, let's go through the house, make sure there's no mold, let's make sure we keep the humidity under 50%," right? Or, "Hey, you got to treat pollen allergy, let's make sure when you come home, you leave your shoes in one place, change your clothes when you get home, don't put those clothes on your bed where you sleep. Make sure you're cleaning off at nighttime, showering or bathing and rinsing your nose to remove all of those pollen grains and potentially irritants too." Depending on where you live, you may have more air pollution. So when there's more travel as we get to warmer months, that means there's going to be more air pollution, that's a non-allergic trigger that could feed into the other allergies that you're experiencing that can lead to these sinus problems.
Gary Falcetano:
Exactly. And I think a lot of people think, well, pollen is everywhere. It's ubiquitous, how do we... And you mentioned some of the techniques that we use, but it's really about the concept of a safe sleep space. And if we can protect that spot where we spend 8, 9, 10 hours a day, the bedroom, it can really have a dramatic impact on symptoms.
Zachary Rubin:
Absolutely. The bedroom is one of the most important places that you have to reduce these different environmental triggers.
Gary Falcetano:
And some of these triggers, as you mentioned, we think about the pollens, the grasses, trees and weeds. In a minute, I'll ask you to maybe speak to when we see tree pollen, grass pollen, weed pollen. But then there's these indoor triggers, we call them perennial triggers. And those are, you mentioned mold, that can be present year round, but also things like dust mites, things like your pets. Whether you live in urban or suburban, mice can be a big issue and we know that can also drive a lot of the symptoms we're talking about. So maybe speak to how once we identify, through testing, what specifically we're sensitized to, how can we address that holistically to reduce symptoms?
Zachary Rubin:
Right, right. So as we mentioned earlier, the bedroom is the first place to start because that's actually where you spend most of your time. So I always tell people make sure you have dustproof covers for your mattress and pillow. If you have carpeting, it's a good idea to remove that if you can afford to and put hardwood floors. If not, you've got to vacuum it at least once a week. And whenever you're dusting, wearing a mask and eye protection can be very helpful because anytime you disturb surfaces, it's going to aerosolize some of those particles that you could be sensitive to. So in the short term, you're trying to help yourself feel better, but then you get some of these symptoms when you're trying to fix that.
Another way to reduce that is to have wet dusting cloths rather than dry. The moisture will help trap some of that. Getting portable HEPA air cleaners or air purifiers for rooms that you spend most of your time in is a good idea. That's especially helpful for things like pet dander.
And I have three dogs. I love my dogs to death, but they do not sleep with me. And I think it's important that people keep their pets out of the bedroom. And I know people don't always like hearing that, but I'd rather say that than say, "Well, we should be getting rid of your animal." And I would never recommend that to my patients. I always say, "Let's find strategies to reduce that." We could say, "Hey, let's bathe your animal regularly." That could actually reduce the amount of allergens that they have. We do want to make sure that when they come from outside, you got to wipe down their paws because they do track a lot of these irritating substances and allergens into the home.
Gary Falcetano:
It's not just people with a dog or a cat allergy, right? But they actually can bring in the pollens from outside or bring in the mold.
Zachary Rubin:
Exactly. So you have to think about all the potential point of contact that come into your home, especially in the bedroom, to mitigate that. And then the one fun thing I like to tell people is if you have a dust mite allergy, there's actually some evidence to show that if you don't make your bed right away, it may help. Because when you make your bed immediately after getting up in the morning, you maintain some of that moisture that your body has generated and it traps it in the bed and increases the dust mite count. So I always say, "Okay, it's okay if you don't make your bed right away, you could do it later." That's [inaudible 00:12:00]-
Gary Falcetano:
Exactly. Let it air out, right?
Zachary Rubin:
Let it air out, exactly.
Gary Falcetano:
That actually brings us to something that's very common, especially with children, especially children that do have asthma. I think a lot of times parents want to put a humidifier in the bedroom to help them breathe a little easier. But if they have a dust mite sensitization or there's mold issues in the house, it's actually like a drinking fountain for the dust mites because that's how they drink. They absorb water from the air.
Zachary Rubin:
Right. Dust mites are roughly what? 80% made of water. They are so reliant on humidity that that's why I was mentioning earlier, keeping the humidity under 50% will decrease the dust mite counts. But at the same time, dry air can irritate the airways too. So it is a balancing act.
In the case of illness, you have to make sure you're cleaning your humidifiers regularly, every other day. It depends on the manufacturer's guidelines on the specific device that you have, but you've got to be cleaning it, otherwise it's going to be an area where mold's going to grow or it's going to allow dust mites to accumulate. But if you also have those dustproof covers, if you are changing sheets regularly and you're vacuuming, dusting, that will help decrease some of those dust mite counts as well.
Gary Falcetano:
Yeah, exactly. And things like maybe not having carpet in the bedroom or washing stuffed animals on a regular basis, or I've even heard putting the stuffed animals in the freezer. [inaudible 00:13:16]-
Zachary Rubin:
Yeah, my mentor in fellowship, he taught me that trick a long time ago. He basically put them in bags, these stuffed animals, leave it in the freezer overnight once a month, and it'll kill off the adult dust mites. But the eggs that they lay, which nobody can really see, that will stay behind. So that's why you have to do that regularly. It is one way to reduce dust mite counts in stuffed animals if, for some reason, you can't get rid of them, A lot of kids are very attached to their stuffed animals. That's one way to safely do that. Granted, do you have the freezer space? That's always a challenge, but it is something that could be potentially helpful.
Gary Falcetano:
Yeah. Yeah. I mentioned the other pollens, tree pollen this time of year, but what about grasses and weeds? And what can we expect as we go through the year?
Zachary Rubin:
When I talk about these things, I'm talking about because I'm in the Chicagoland area, so every region's a little bit different. You look at Texas, they have cedar fever in December, January, and that tree pollen from Ash junipers coming out and people are miserable in the winter time. But for a lot of other parts of the country, you start seeing pollen being released in March. So that's tree pollen, March, April, May. And then as we transition from May into June, it goes into the grass pollen months, which is the shortest season out of the three, so that's usually around June, July. And then as we get into late July, August, the weed pollens come out up until that first hard frost in your area. Once that hard frost happens, the pollen will stop.
Gary Falcetano:
And we're starting to see some overlap. It's kind of controversial to talk about the warming climates, but we're starting to see overlaps where spring tree pollen season may be starting a little earlier, extending into or overlapping with grass pollen. So sometimes it's hard, just based on the time of the year, to figure out what exactly you're sensitized to.
Zachary Rubin:
Yeah, that's why it's important to look at the pollen counters in your area. As an example, the American Academy of Allergy, Asthma, and Immunology, or Quad AI, they have a pollen counter in many major cities that you can subscribe to and they'll give you morning emails to tell you what's going on. I'm hoping in the future we'll have better technology to get more real-time estimates because really, you got to hand count a lot of this. These manual counters, it's very labor-intensive. I know there's a lot of work done to make more accurate automated systems so that we know more in real time what's going on.
But as a rule of thumb, if it's dry and windy, you see that in the forecast, the pollen counts are likely going to be higher. If it's going to be raining, the pollen counts will be lower, but the mold counts will be higher because mold follows moisture. So those are some general rules of thumb for people to think about when trying to manage their allergies.
Gary Falcetano:
Yeah, absolutely. So we've talked about the preventative medicine exposure reduction techniques that we can use when we're sensitized, but we also probably should talk a little bit about medications. And maybe you can speak to that concept of priming and identifying when we think, based upon our sensitizations and when pollen counts are going to be high, how we can prevent getting into the thick of symptoms.
Zachary Rubin:
Right, exactly. So this is especially true for pollen allergies, the seasonal allergic rhinitis patients. If you don't start your medications early enough, it's harder to treat because once you start getting that exposure, the inflammation that occurs will just keep getting worse, worse, worse, and worse and worse. That's the basic concept of what you mean by priming in that sense.
So if you know that pollen season is going to start roughly the first couple of weeks in March, you should be starting your medicine two to four weeks before then because that gives your body enough time to get used to the medication, it builds up in your system, especially for nasal steroid sprays like fluticasone, mometasone, triamcinolone, your Flonase, Nasacort, Nasonex, over-the-counter sprays. If you're doing that two to four weeks ahead of time, then you have really helped cut off that potential priming stage to reduce the chances of having significant symptoms.
If you start your medicine in April, you're playing a lot of catch-up and it's going to take so much more time, and you're higher risk of having sinus infections, ear infections, problems sleeping at night, which sleep is such a premium and such an important part of our health. We can't concentrate as well, our blood pressure goes up if we don't sleep well, our weight goes up, cholesterol issues. So sleep is so important. That's why I'm so passionate about my specialty is because we're a type of niche specialty that helps people improve not only their quality of life, but indirectly their quantity of life as well.
Gary Falcetano:
Yeah, absolutely. So we have a couple of questions coming in, and I think we answered one of them, but this is probably a Nobel Prize winning, if you can answer this, right?
Zachary Rubin:
Uh-huh.
Gary Falcetano:
We know allergies change over time. What's the hypothesis there on why, particularly young children will develop more allergies, they'll develop tolerance to food allergies as they age? Why do our allergic responses really change?
Zachary Rubin:
Yeah, so the short end of it is we don't know, obviously. As you said, this would win a Nobel Prize if we could fully understand this because there are people out there who will have a cat allergy and randomly one day not be allergic. And we have no idea what was the trigger that caused that to happen. We have bits and pieces of the story put together in terms of we know that, like I mentioned in the beginning of our session together, is that Ig antibodies are produced. They're produced by specific cell called B cells, and there's a whole process called sensitization happening, but we don't know sometimes what the initial inciting factor is. It's probably a complex interplay between genetics and environment that's doing this.
So the environmental triggers of how that happens is not fully understood, but we know that there are more and more people developing these problems over time, starting in childhood and going into adulthood, especially correlating with, we have higher pollen counts, we have more air pollution in certain areas. There's certain exposures that we know have increased over time, and that's correlated positively with more people being diagnosed with these problems. It's why I hear every single year, "Why are my allergies worse this time than last year? Why is it the worst this year compared to any other year?" Well, you're exposed more to these problems that are causing the allergic symptoms. Part of why people later in life may see less allergy symptoms is the immune system just gets weaker as we age. So we know that.
Gary Falcetano:
Immunosenescence, I believe is the term.
Zachary Rubin:
Exactly.
Gary Falcetano:
Right? Yeah.
Zachary Rubin:
Exactly. Yes. But not everybody does that. And then on the flip side too, you may lose your allergic rhinitis where your immune system is sensitized and that allergy antibody is present. But then the anatomy changes and some of the immune system changes, and you develop non-allergic rhinitis. So as you get older, a lot of times people will have a runny nose that's running like a faucet. And that's more of a structural mechanical problem rather than an immune system problem.
Gary Falcetano:
And you need to rule out allergy first, what we mentioned, called phenotyping. Is this an allergic mechanism or is it a non-allergic? And then when it's non-allergic, going down that clinical pathway to figure out exactly what it is.
Zachary Rubin:
Exactly.
Gary Falcetano:
Yeah.
Luke Lemons:
Thank you for listening today, and I hope you enjoyed this conversation with Dr. Rubin on Allergy Insider. Again, they're great patient education. They've got articles on their webpage around specific allergies. They have a bunch of content on their Instagram. And the goal really is to make sure that patients are getting the most medically accurate allergy information out there online.
If you want to learn more about some of the pitfalls of online education and social media, Dr. Rubin again does a great episode on this on ImmunoCAST. That's episode 24, called Navigating Social Media as a Clinician. And if you want to hear Gary and I talk through the symptom threshold with more of a clinician lens, we have an episode around that as well, that is episode two.
All this will be linked on this episode's page via the link in the description. Thank you for listening.
Announcer:
ImmunoCAST is brought to you by Thermo Fisher Scientific creators of ImmunoCAP Specific IgE Diagnostics and Phadia Laboratory Systems. For more information on allergies and specific IgE testing, please visit ThermoFisher.com/immunocast. Specific IGE testing is an aid to healthcare providers in the diagnosis of allergy and cannot alone diagnose a clinical allergy. Clinical history alongside specific IgE testing is needed to diagnose a clinical allergy. The content of this podcast is not intended to be, and should not be interpreted as or substitute, professional medical advice, diagnosis, or treatment. Any medical questions pertaining to one's own health should be discussed with a healthcare provider.
- Cox L, Williams B, Sicherer S, Oppenheimer J, Sher L, Hamilton R, Golden D; American College of Allergy, Asthma and Immunology Test Task Force; American Academy of Allergy, Asthma and Immunology Specific IgE Test Task Force. Pearls and pitfalls of allergy diagnostic testing: report from the American College of Allergy, Asthma and Immunology/American Academy of Allergy, Asthma and Immunology Specific IgE Test Task Force. Ann Allergy Asthma Immunol. 2008 Dec;101(6):580-92.
- Calderón MA, Cox L, Casale TB, Moingeon P, Demoly P. Multiple-allergen and single-allergen immunotherapy strategies in polysensitized patients: looking at the published evidence. J Allergy Clin Immunol. 2012 Apr;129(4):929-34.
- Wickman M. When allergies complicate allergies. Allergy. 2005;60 Suppl 79:14-8.
- Lopez CM, Yarrarapu SNS, Mendez MD. Food Allergies. 2022 Mar 15. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 29489188. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482187/.
- Smith HE, Hogger C, Lallemant C, Crook D, Frew AJ. Is structured allergy history sufficient when assessing patients with asthma and rhinitis in general practice? J Allergy Clin Immunol. 2009 Mar;123(3):646-50.
- Bousquet J, Anto J M et al. Allergic rhinitis. Nat Rev Dis Primers 2020;6(1):95.
- Scadding G K, Scadding G W. Diagnosing allergic rhinitis. Immunol Allergy Clin North Am 2016;36(2):249-260

Legal manufacturer: Phadia AB.
Before you proceed ...
We noticed you may be visiting a version of our website that doesn’t match your current location. Would you like to view content based on your region?
Talk with us
Interested in utilizing our solutions in your laboratory or healthcare practice?
This form is dedicated to healthcare and laboratory professionals who work within medical laboratories, private practices, health systems, and the like.
By clicking "continue with form" you are confirming that you work within a healthcare or laboratory space.
Not a lab professional or clinician but interested in diagnostic testing for allergies?
Visit Allergy InsiderChoose your preferred language
Please note: By selecting a different language, you are choosing to view another site. Product availability and indications may vary from what is approved in your region.