In the early 2000s, clinical trials were underway for the drug Cetuximab to treat colorectal cancer and head and neck cancers. Patients began having reactions to the drug and after some investigation, researchers identified that an allergic reaction was taking place to the oligosaccharide galactose-α−1,3-galactose, known as alpha-Gal, contained in the medication.1
Around the same time, patients presenting odd reactions after eating red meat were seen in similar regions where the Cetuximab reactions took place. The medical mystery was solved when researchers determined that the lone star tick (Amblyomma americanum) can transfer alpha-Gal to humans via a bite.1

Ticks pick up the alpha-Gal molecule from feeding on deer or other mammals and then transfer it to humans when they bite them. Although it can take months, the human body then has an immune response to the alpha-Gal when it’s ingested later in red meat.1 When humans have an IgE response to alpha-Gal, it can lead to severe reactions after eating red meat and organ meats (i.e., beef, pork, lamb, organs), milk, and even some non-meat products made from parts of mammals, like medications and gelatin.2
This "alpha-gal allergy," known as alpha-Gal syndrome (AGS), has been diagnosed in the U.S. and regions all over the world, yet it’s still relatively unknown and functions in unusual ways compared to other allergies. Here are important facts to familiarize yourself with this allergic condition.
A paradigm shift for allergy diagnosis
Not only does AGS begin differently than other allergies, it presents in unusual ways as well. Unlike other food allergies that begin immediately or within two hours of ingestion, AGS symptoms usually start 3-6 hours after eating red meat.2 Symptoms can include itching, hives, or sometimes even anaphylaxis, but they also frequently include gastrointestinal symptoms like abdominal pain, vomiting, and diarrhea.2
For patients, going into anaphylactic shock hours after consuming a meal can be bewildering and it doesn’t seem like a food allergy. Complicating things even further, in many cases patients only have gastrointestinal symptoms. That can seem like food poisoning, instead of an allergic reaction, when they occur hours after eating.1 In all cases, these conditions make it confusing for patients and providers alike to pinpoint what is going on.
Specific IgE allergen component tests are crucial for confirmation
Skin-prick tests for AGS are unreliable, and it is recommended that specific IgE blood testing be used to identify the presence of alpha-gal.1 This alone is not enough for a diagnosis. Patient history, particularly exposure to tick bites, is critical.
That history paired with the results of a specific IgE blood test and clinical response to red meat consumption are important for diagnosis.1 Specific IgE blood testing is therefore part of confirming a diagnosis — it shouldn’t be used for screening purposes. Why not? Because certain populations, particularly in rural areas, may show high incidences of alpha-Gal present in blood samples, yet most people in those populations have no symptoms while eating red meat at all.3 This is why a multi-faceted examination is needed for an accurate diagnosis.
You can always find the most up-to-date allergen test codes with alpha-Gal allergen profiles in the Lab Ordering Guide.
Additional 'alpha-Gal allergy' factors to watch for
There is still much to learn about alpha-Gal Syndrome, but more information is coming to light all the time. There are multiple factors that can play a role in how severe reactions are and how long the condition lasts in patients.
Alcohol and exercise can intensify symptoms
In a recent study, approximately one-third of patients reported that drinking alcohol (29%) or exercise (32%) increased reaction severity.4 These are factors to keep in mind when discussing patient history — did the patient drink a glass of wine with a steak dinner, or did they work out prior to eating at a barbeque? Not only is this information useful when making a diagnosis, it's also important for patients to understand the connections between these seemingly unrelated events.
It's not just meat that can cause reactions
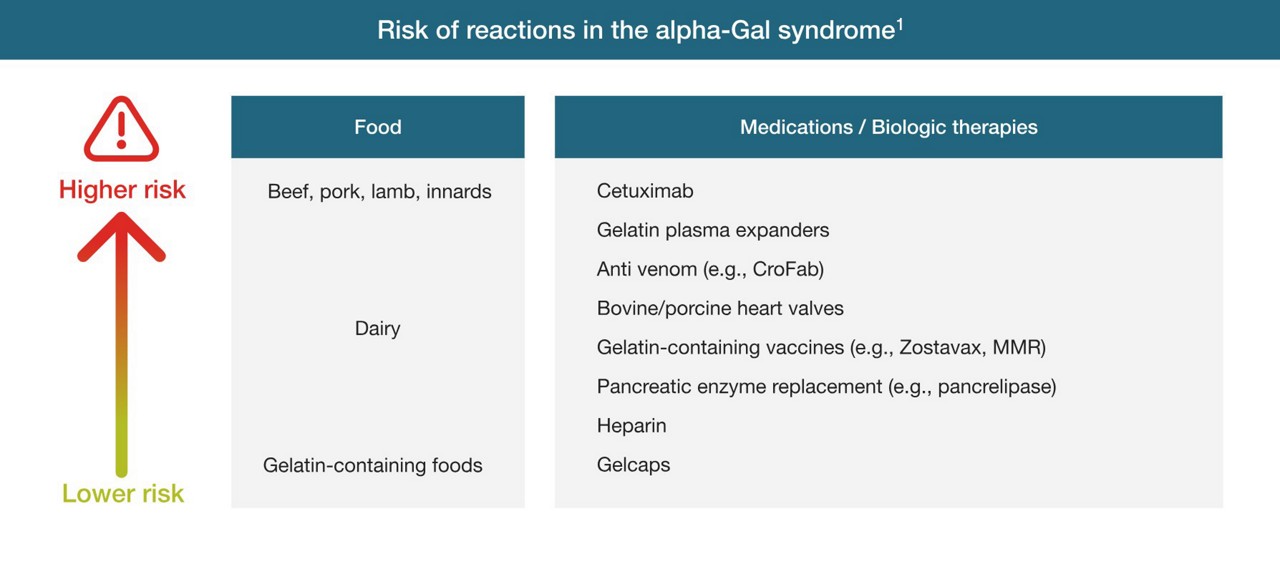
The main strategy for managing alpha-Gal syndrome is avoidance of beef, pork, lamb, and other mammalian meats such as venison, organ meats or organ casings.3 Depending on the patient, dairy products may also need to be avoided as they also contain lower amounts of alpha-Gal.
Gelatin, which is made from collagen from mammals, can also cause reactions.1 Gelatin is present in candies and marshmallows but also in medication or vitamin supplement capsules.1 It’s also present in some vaccines and pancreatic enzyme replacements.1 Even bovine or porcine heart valve replacements can cause reactions, so patients undergoing these intensive interventions should be thoroughly evaluated for AGS.1
The risk and severity of reactions in alpha-Gal syndrome are influenced by the oligosaccharide quantity in food, drugs or therapeutics. Administration route matters, as intravenous exposure triggers rapid reactions, while oral ingestion leads to delayed onset.
Patients with group B blood have a lower rate of sensitization
Studies have shown that patients with type B or AB blood are less likely to have measurable alpha-Gal specific IgE antibodies.3 The reason isn’t fully understood yet, but alpha-Gal is closer in structure to type B than to types A or O, so it’s possible that patients with type B blood are less likely to produce an antibody to a similarly structured carbohydrate.3
Tick bite prevention is key clinical advice
There isn’t a cure for alpha-Gal syndrome, but avoiding tick bites is the most important factor. Patients may see sharply reduced amounts of alpha-Gal in their bloodstream over time and eventually be able to eat mammalian meats again.1 But, if they are bitten again by a tick, it can maintain or increase their alpha-gal levels.1
Guidance on wearing protective clothing and using bug spray is therefore very important for patient care. And, as deer populations migrate, this advice will become valuable for patients everywhere, not just in areas where the lone star tick has historically been found. In fact, U.S.-based researchers first identified AGS as connected to lone star tick populations in the American Southeast (not in Texas, despite the insect’s name).1 But lone star ticks are moving into other regions, as far north as Maine and as far west as Nebraska.5 As deer migrate and winters become warmer due to climate change, the ticks move with them and can survive in areas where previously they could not.5
It’s very important to ask patients who have experienced an immune response to alpha-Gal if they have traveled within the last few months to a hotspot like the Southeast, but geography is not the only determining factor as tick populations move and spread. As evidenced by AGS cases on different continents, it’s also clear that the lone star tick also isn’t the only insect vector for this condition.