Allergic rhinitis: how to identify the primary sensitisation
David, a 20-year-old university student based in Manchester, presents to his GP in mid-July with a 3-month history of rhinorrhoea, nasal congestion, itching, and sneezing. He also has sore, red, and itchy eyes, and has been sleeping poorly. When questioned about his mood, David confesses that he is very worried about his upcoming exams, and how his health may affect his performance.
Find out how the primary sensitisation was identified with the aid of a simple blood test.
Patient history
Personal history
David was previously diagnosed with seasonal allergic rhinitis at the age of 16. He first noticed his symptoms in May, and they were at their worst in July. At the age of 18, he was diagnosed with mild depression.
Medication history
- Previously trialled intranasal antihistamines, which were ineffective at controlling his nasal symptoms
- Currently prescribed an antihistamine/cortisone combination intranasal spray
Examination, investigations, and results
Examination
Whilst talking to David, his GP noticed that he had nasal speech, and was frequently sniffing and rubbing his nose. Allergic shiners were observed upon close inspection of his face, and internal examination of his nose revealed turbinate hypertrophy.
Examination and auscultation of David’s chest revealed no obvious abnormalities or stigmata of asthma.
Which of David’s symptoms are particularly suggestive of allergic rhinitis, as opposed to non-allergic rhinitis?
Manifestations of rhinitis, which are particularly suggestive of allergy, are:1
- Itchy nose and/or palate
- Sneezing
- Eye-related symptoms
Investigations
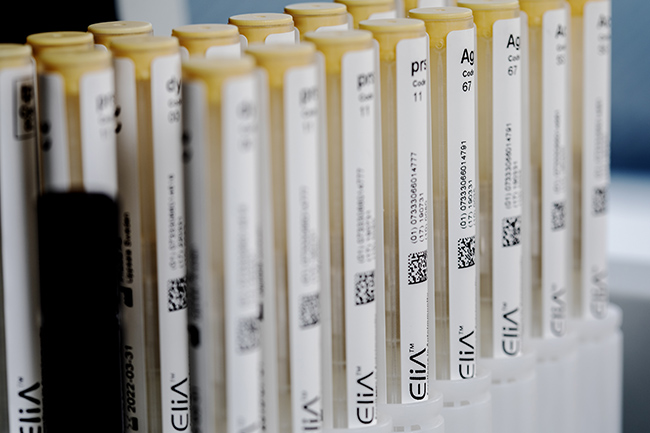
David’s GP decided to request a specific IgE blood test; SPTs are contraindicated in patients who have recently taken antihistamines, and David did not wish to discontinue his medication.1 The panel of allergens was selected based on David’s symptoms, age, and local sensitisation patterns. As his symptoms usually begin in May and are at their worst in July, a range of allergens that typically present in spring/summer (including pollens and a fungus), were selected for testing.
Test* |
Type |
David’s Results |
| Timothy grass (g6) | Whole allergen |
38 |
| Silver birch (t3) | Whole allergen |
<0.10 |
Common ragweed (w1) |
Whole allergen |
<0.10 |
| Mugwort (w6) | Whole allergen |
<0.10 |
| Alternaria alternata (m6) | Whole allergen |
<0.10 |
How could these specific IgE blood test results guide the GP’s management of David?
Specific IgE blood test results could guide the GP’s management of David in various ways, including:2,3
- Confirmation of his previous seasonal allergic rhinitis diagnosis
- Determination of appropriate pharmacotherapy and timing of therapy
- Guidance on local allergen avoidance strategies
- Consideration of allergen immunotherapy†
†Refer to specialists/allergists for allergen immunotherapy, if required.
Differential Diagnosis
The results showed a significant IgE response to Timothy grass, confirming the previous diagnosis of seasonal allergic rhinitis. No other sensitisations were found, so allergies to birch pollen, ragweed, mugwort, and Alternaria alternata can be ruled out.
Management
As Timothy grass is an outdoor allergen, it cannot be completely avoided.4 However, David could use the following techniques to help limit his exposure:5
- Keep windows closed during pollen season.
- Check Timothy grass pollen counts. In spring and summer, levels are highest in the evening.
- Take a shower, wash hair, and change clothing after working or playing outdoors.
Information gained from specific IgE blood tests can be an important factor in deciding on the best pharmacotherapy. For example, commencing therapy just before the start of the local grass pollen season could maximise treatment effectiveness for David.2
Allergen immunotherapy (AIT) is the only potentially disease-modifying option for the treatment of allergies,6 and is usually initiated by allergy specialists.7 Appropriate AIT can prevent the development of asthma8 and, in patients with comorbid asthma, improve symptom control.9 David’s GP decided to refer him to an allergy specialist for selection of AIT.
*The following products are included in the ImmunoCAP™ blood test range:
- ImmunoCAP Allergen g6, Timothy
- ImmunoCAP Allergen t3, Common silver birch
- ImmunoCAP Allergen w1, Common ragweed
- ImmunoCAP Allergen w6, Mugwort
- ImmunoCAP Allergen m6, Alternaria alternata
IgE : immunoglobulin E; kUA/L: allergen-specific kilo units per litre
The people, places, and events depicted in these case studies and photographs do not represent actual patients, nor are they affiliated in any way with Thermo Fisher Scientific.
- Scadding G K, Scadding G W. Diagnosing allergic rhinitis. Immunol Allergy Clin North Am 2016;36(2):249-260
- Eigenmann P A, Atanaskovic-Markovic M et al. Testing children for allergies: why, how, who and when: an updated statement of the European Academy of Allergy and Clinical Immunology (EAACI) Section on Pediatrics and the EAACI-Clemens von Pirquet Foundation. Pediatr Allergy Immunol 2013;24(2):195-209
- Bousquet J, Anto J M et al. Allergic rhinitis. Nat Rev Dis Primers 2020;6(1):95
- Roberts G, Xatzipsalti M et al. Paediatric rhinitis: position paper of the European Academy of Allergy and Clinical Immunology. Allergy 2013;68(9):1102-1116
- American College of Allergy A I. Environmental trigger avoidance. Available at: https://acaai.org/allergies/allergy-treatment/environmental-trigger-avoidance. Accessed March 2022
- Pfaar O, Klimek L et al. COVID-19 pandemic: practical considerations on the organization of an allergy clinic-an EAACI/ARIA position paper. Allergy 2021;76(3):648-676
- Bousquet J, Pfaar O et al. 2019 ARIA care pathways for allergen immunotherapy. Allergy 2019;74(11):2087-2102
- Jacobsen L, Niggemann B et al. Specific immunotherapy has long-term preventive effect of seasonal and perennial asthma: 10-year follow-up on the PAT study. Allergy 2007;62(8):943-948
- Bergeron C, Hamid Q. Relationship between asthma and rhinitis: epidemiologic, pathophysiologic, and therapeutic aspects. Allergy Asthma Clin Immunol 2005;1(2):81-87