Celiac disease versus IBS: is it really such a clinical conundrum?
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed mattis finibus tincidunt. Quisque sollicitudin pretium ligula, cursus consequat est tempor a.
Vivamus vitae diam malesuada, iaculis ligula vitae, vulputate tortor. c cursus interdum. Suspendisse interdum ornare
Gemma, a 30-year-old woman from Windsor, had been suffering with ill health for over a decade by the time she attended an appointment with her GP in July 2018.
2002-2005
Aged 14-17 years, Gemma had multiple presentations to primary care, due to abdominal cramping and stomach upset in connection with food intake. At this time, the GP advised her to ensure she ate a healthy and varied diet, including plenty of fibre.
2007
At the age of 19 years, Gemma presented to her GP again, with difficulty eating, abdominal pain, mild diarrhoea, and general malaise/fatigue. Her full blood count and haematinics were normal, and she was referred for a colonoscopy which did not discover any abnormalities. The GP told Gemma that the most likely cause of her symptoms was irritable bowel syndrome (IBS), and no further investigations were performed.
Gastrointestinal symptoms alone cannot accurately differentiate celiac disease from IBS;1 organic diseases such as celiac disease should be ruled out before a diagnosis of IBS is made.2
Celiac disease has a prevalence of 1 percent in the general population,3 and up to 4.7 percent in patients who were diagnosed with IBS based on symptom criteria.4
2011-2017
Between the ages of 23 and 29 years, Gemma had three complicated pregnancies. With all three, she suffered with intense pruritis during the last two trimesters, with very high levels of serum bilirubin and alanine aminotransferase. Intrahepatic cholestasis of pregnancy was determined to be the cause, and the pruritis spontaneously resolved in the postnatal period. All three children were born prematurely.
Celiac disease is associated with high miscarriage rates, intrauterine growth retardation, low birth weight, and preterm birth.5
July 2018
By the time of her GP appointment in July 2018, Gemma had been struggling with her bowel symptoms for the past 11 years.
Gemma, aged 30 years: “The pain and disease fill so much of my everyday life.”
Over the years, Gemma's symptoms had evolved; she now had a very poor appetite, weight loss, and rashes and blister-like lesions on her elbows.
Gemma's GP ordered thyroid function tests and checked her vitamin D levels.
| Test | Gemma's results |
|---|---|
| Thyroid-stimulating hormone (TSH) | high (5.2 mU/L) |
| Free thyroxine (FT4) | lower limit of normal (12 pmol/L) |
| Vitamin D | low (18 nmol/L) |
The GP postulated that Gemma’s vitamin D deficiency could be the reason for many of her symptoms and prescribed once-daily cholecalciferol capsules (1,400 IU).
January 2019: 6-month follow-up appointment
6 months later, Gemma’s TSH was still mildly elevated, her FT4 was still on the lower limit of normal, and her vitamin D levels had returned to normal. Given that she no longer had vitamin deficiency, which was thought to be the cause of her illness, she felt pressured to ‘feel better’. However, her symptoms had not improved.
Gemma:
- Slept 9-10 hours every day
- Had dry, blistery skin on her elbows
- Suffered with depression and stress
Despite all this, she had become so used to her poor toilet habits that she no longer noticed them; they had become part of her everyday life.
Around this time, Gemma began to keep a diary, and realised that her symptoms seemed to be linked to food consumption, but with no clear pattern of what food they might have been related to.
July 2019: 6 months later, Gemma presented to primary care again
At the age of 31 years, Gemma's bowel habits had significantly worsened, triggering a return to her GP. She showed the GP the diary which she had been keeping, after which the GP decided to test for celiac disease and food allergy. As she also had a history of mildly elevated TSH, the GP added in a test for autoimmune thyroid disease.
Gemma’s blood results were as follows:
| Test | Gemma's results |
|---|---|
| Tissue transglutaminase (tTG) IgA | positive (118 U/mL, 12x ULN) |
| Total IgA | normal (2.1 g/L) |
| Specific IgE to a panel of food allergens, including wheat | negative (<0.1 kAU/L) |
| Anti-thyroid peroxidase (TPO) antibodies | positive (2,400 IU/mL) |
tTG IgA is the recommended first-line test for celiac disease, together with total IgA to check for IgA deficiency.6
New diagnosis
Based on the results of her most recent blood tests and following confirmation by a gastroenterologist, Gemma's primary diagnosis was changed from IBS to celiac disease. Gemma was advised to begin a strict gluten-free diet, and to carry on keeping her diary—taking particular care to log food and symptoms.
Gemma, aged 31 years: “Finally there is a blood test that can answer some of the many symptoms I have had for many years.”
It takes, on average, 10-13 years to receive a correct diagnosis of celiac disease.7,8
September 2019
Gemma's endocrinologist ran further thyroid-function and antibody tests and found that she had subclinical Hashimoto's thyroiditis. This did not require treatment but was to be reviewed on a 3-monthly basis.
The prevalence of celiac disease in patients with autoimmune thyroid disease is 2-5 percent.9
July 2020
By mid-2020, Gemma had completed 1 year of a strict gluten-free diet. Her bowel habits were much improved, but she still suffered with muscle pain, dry skin, malaise/fatigue, and depression.
Her tTG IgA levels were falling (43 U/mL, 4x ULN), but TSH was still elevated and FT4 had dropped below the lower limit of normal. She was subsequently diagnosed with hypothyroidism secondary to Hashimoto's thyroiditis, and began treatment with levothyroxine.
It is common practice for tTG IgA to be tested every 3 months, until normalised, and once a year as an indicator of diet adherence.6
September 2020: Following 2 months of treatment
Following 2 months of treatment with levothyroxine, Gemma's:
- TSH was improving and FT4 normalised
- Muscle pain was almost gone
- Fatigue and depression were resolved
Gemma, aged 32 years: “I am relieved to finally feel I have received answers to the inconveniences and the malaise. But, at the same time, I feel despair and frustration, and have a lot of unanswered questions. Have I had it for a long time? So, I have REALLY been sick—despite previously coming to the conclusion that it had to be something mental and not physical.”
COMING SOON
Case study 3: Coeliac disease or IBS?
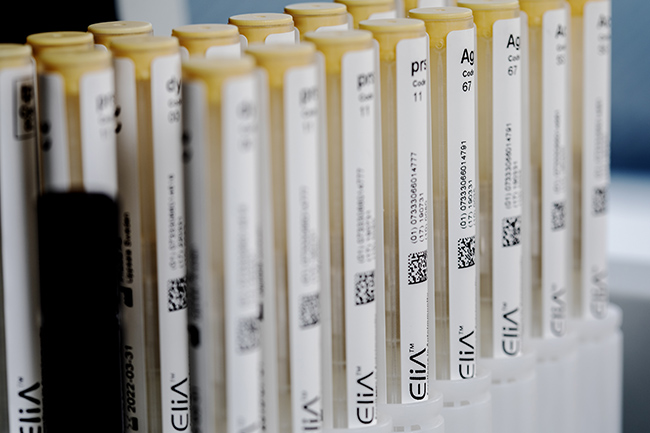
<Name> ImmunoCAP™ Test Results
These results together with this patient's case history and symptoms, help confirm the diagnosis.
| Test | Type | <Patients Name> Results |
| Test Name | Whole or Component | ## |
- Rubio-Tapia A, Hill I D et al. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol 2013;108(5):656-676;quiz 677
- Moayyedi P, Mearin F et al. Irritable bowel syndrome diagnosis and management: a simplified algorithm for clinical practice. United European Gastroenterol J 2017;5(6):773-788
- Gujral N, Freeman H J, Thomson A B. Celiac disease: prevalence, diagnosis, pathogenesis and treatment. World J Gastroenterol 2012;18(42):6036-6059
- El-Salhy M, Hatlebakk J G et al. The relation between celiac disease, nonceliac gluten sensitivity and irritable bowel syndrome. Nutr J 2015;14:92
- Shah S, Leffler D. Celiac disease: an underappreciated issue in women's health. Womens Health (Lond) 2010;6(5):753-766
- Al-Toma A, Volta U et al. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United European Gastroenterol J 2019;7(5):583-613
- Gray A M, Papanicolas I N. Impact of symptoms on quality of life before and after diagnosis of coeliac disease: results from a UK population survey. BMC Health Serv Res 2010;10:105
- Norström F, Lindholm L et al. Delay to celiac disease diagnosis and its implications for health-related quality of life. BMC Gastroenterology 2011;11(1):118
- Ch'ng C L, Jones M K, Kingham J G. Celiac disease and autoimmune thyroid disease. Clin Med Res 2007;5(3):184-192

Before you proceed ...
We noticed you may be visiting a version of our website that doesn’t match your current location. Would you like to view content based on your region?
Contact us
Interested in utilizing our solutions in your laboratory or healthcare practice?
Not a lab professional or healthcare provider but would like to learn more about allergy testing?
Visit Allergy InsiderChoose your preferred language
Please note: By selecting a different language, you are choosing to view another site. Product availability and indications may vary from what is approved in your region.