Cow’s milk allergy diagnosis:
a step-by-step guide
About cow’s milk allergy (CMA)
CMA is the leading cause of food allergy in children under 3 years of age but may be diagnosed in patients of all ages. As symptoms of CMA overlap with those of other gastrointestinal disorders, appropriate diagnostic workup is vital to avoid over- and under-diagnosis, and thus minimise the health burden to patients and their families.1
Read through this evidence-based guide to learn how to accurately diagnose CMA in clinical practice.
Steps 1-2: primary care
1. Medical history and physical examination
The symptoms of CMA can be diverse and of variable intensity, involving many different organ systems, but most commonly the skin and the gastrointestinal and respiratory tracts. The involvement of ≥2 systems increases the likelihood of CMA.1
Immediate and delayed reactions should be differentiated; however, combinations of these two types of reaction may be present in one patient.1
- Immediate reactions: occur from minutes up to 2 hours after allergen ingestion and are more likely to be IgE-mediated.1
- Delayed reactions: manifest up to 48 hours following ingestion.1
If any of the following signs or symptoms occur in an infant or child, and cannot be explained by another cause, CMA may be considered a potential diagnosis:1
- Cutaneous: urticaria, angio-oedema, exacerbation of atopic dermatitis
- Gastrointestinal: dysphagia, gastro-oesophageal reflux, colic, abdominal pain, vomiting, anorexia, diarrhoea, blood in stools, constipation, iron deficiency anaemia
- Respiratory: rhinorrhoea, wheeze, chronic cough, difficulty breathing
- General: anaphylaxis, shock-like symptoms,* failure to thrive
*Anaphylaxis or shock-like symptoms are clear indications for a referral to an allergy specialist.
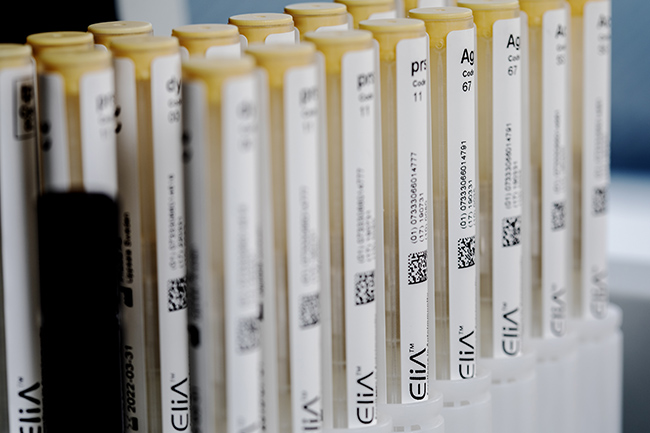
2. Laboratory tests such as specific IgE blood tests
If the patient’s history indicates IgE-mediated allergy, specific IgE blood tests can assist in the diagnosis.2,3 Specific IgE blood tests can be performed at any age and use validated assays to quantify allergen-specific IgE levels in the serum.2 Firstly, a test for a specific IgE response to the whole allergen (cow’s milk) should be performed.3
Interpretation of whole-allergen specific IgE blood test results1
- Results should always be interpreted in the context of the patient’s clinical history.
- The presence of a specific IgE response to cow’s milk indicates a sensitisation to cow’s milk, and an associated IgE-mediated immunological process.
- The higher the antibody titre, the greater the probability of having CMA, and allergy persistence.
- Children with gastrointestinal manifestations of CMA are more likely to have negative results than those with cutaneous manifestations, but a negative test result does not exclude CMA.
Whole-allergen tests predict the likelihood of CMA but are not predictive of reactivity to baked milk. After testing for a specific IgE response to whole allergen, cow’s milk allergen component tests can help evaluate reactivity to baked goods and provide further information on the likelihood of allergy persistence.3
Assessment of specific IgE responses to the following components (proteins) could help pinpoint the diagnosis and guide the management of patients with CMA:3
- Alpha-lactalbumin (f76 / nBos d 4)
- Beta-lactoglobulin (f77 / nBos d 5)
- Bovine serum albumin (e204 / nBos d 6)
- Casein (f78 / nBos d 8)
As caseins are more resistant than other proteins to heat denaturation, patients with high levels of casein-specific IgE are likely to react to baked milk. Such patients should therefore avoid consumption of all forms of milk. Patients who test negative for casein-specific IgE may be able to tolerate extensively heated milk, for example in baked goods.3
70-80 percent of children with CMA do not react to milk in baked products.3
Consider using allergen component blood tests to identify these patients.3
Steps 3-6: secondary care
3. Diagnostic elimination diet
If relevant symptoms are present and CMA is likely, a diagnostic elimination diet should be initiated. Cow’s milk should be strictly excluded from the patient’s diet (or the mother’s diet in case of breastfeeding) for a limited period.1
The duration of the elimination diet should be kept as short as possible whilst being long enough to judge whether clinical symptoms resolve or stabilise. The required duration may be:1
- 3-5 days in patients with immediate reactions
- 1-2 weeks in patients with delayed reactions
- 2-4 weeks in certain other patients (e.g., those with chronic diarrhoea or failure to thrive)
If no improvement in symptoms is seen, then CMA is unlikely. However, exceptions may occur, especially in cases of multiple sensitisations. Infants with significant gastrointestinal symptoms that do not improve when using a hydrolysed or soy formula may benefit from a trial of an amino acid-based formula before CMA is excluded.1
4. Oral food challenge
If symptoms significantly improve during the diagnostic elimination diet, the diagnosis of CMA should be confirmed by a standardised oral food challenge (OFC) under medical supervision.1
In cases of anaphylactic/clear immediate reaction to cow’s milk and a positive whole-allergen specific IgE blood test, cow's milk should be strictly excluded from the diet (see step 5) and the OFC can be omitted. Cow's milk should be excluded from the diet for at least 1 year before an oral food challenge is considered by a specialist.1
If an immediate reaction to cow’s milk is apparent but the whole-allergen specific IgE blood test is negative, an OFC should be carried out in a hospital setting under strict medical supervision.1
5. Strict exclusion of cow's milk from the diet
Strict avoidance of cow's milk is the safest strategy in the management of CMA. Cow's milk should be eliminated from the diets of patients with:1
- A diagnosis of CMA confirmed by an OFC, or
- A history of an anaphylactic/clear immediate reaction to cow’s milk, and positive whole-allergen specific IgE blood test
Based on allergen component blood test results, patients may be able to tolerate extensively heated (baked) milk. Dietary inclusion of baked products containing cow’s milk may accelerate development of tolerance to unheated cow’s milk.3
6. Re-evaluation at 6-12 months
Patients should be re-evaluated at around 6-12 months, to avoid continuing the restrictive cow's milk exclusion diet for an unnecessarily long time.1,3 The nutritional benefits of cow’s milk are well known, and restrictions on its intake, particularly in childhood, may result in stunted growth.1 Periodic re-assessments with laboratory tests and oral food challenges are recommended.3
IgE: immunoglobulin E
- Koletzko S, Niggemann B et al. Diagnostic approach and management of cow's-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines. J Pediatr Gastroenterol Nutr 2012;55(2):221-229
- Eigenmann P A, Atanaskovic-Markovic M et al. Testing children for allergies: why, how, who and when: an updated statement of the European Academy of Allergy and Clinical Immunology (EAACI) Section on Pediatrics and the EAACI-Clemens von Pirquet Foundation. Pediatr Allergy Immunol 2013;24(2):195-209
- Matricardi P M, Kleine-Tebbe J et al. EAACI molecular allergology user's guide. Pediatr Allergy Immunol 2016;27 Suppl 23:1-250

Before you proceed ...
We noticed you may be visiting a version of our website that doesn’t match your current location. Would you like to view content based on your region?
Contact us
Interested in utilizing our solutions in your laboratory or healthcare practice?
Not a lab professional or healthcare provider but would like to learn more about allergy testing?
Visit Allergy InsiderChoose your preferred language
Please note: By selecting a different language, you are choosing to view another site. Product availability and indications may vary from what is approved in your region.