Autoimmune diseases are a growing health concern.1,2 Polyautoimmunity—where patients present with more than one autoimmune disease3—highlights the relevance of general practitioners (GPs) to intervene in the time to diagnosis and quality of life management.4,5 This article underscores their critical role in identifying and managing these patients, particularly in aiding secondary care specialists to identify concurrent autoimmune diseases through case finding.

Why are general practitioners critical for patients who may have polyautoimmunity?
High prevalence: Polyautoimmunity is not just a clinical curiosity; it is a significant aspect of patient care that demands attention.6,7 Recent studies reveal that polyautoimmunity is more prevalent than previously described.8 Specifically, estimates indicate that about 25% of patients with one autoimmune condition are likely to develop additional autoimmune diseases.6 This underlines the need for increased vigilance among GPs.
Overlapping symptoms: Patients with polyautoimmunity often present with overlapping symptoms, which can complicate the time to diagnosis and disease management.4
Early intervention: Prompt and accurate diagnosis with appropriate treatment can improve patient outcomes and prevent significant morbidity and further damage to the body.2,9 GPs, as the first point of contact, play a pivotal role in early identification and in accurate and timely referral to secondary care.5,10
By intervening early, GPs can help prevent serious complications.
Autoimmune disease |
Impact of early intervention |
|---|---|
| Autoimmune thyroid diseases: Graves' disease, Hashimoto's thyroiditis | Reduces likelihood of severe secondary conditions, improving patient outcomes11 |
| Coeliac disease | Reduces risks of malnutrition and osteoporosis12 |
| Inflammatory bowel diseases: Crohn's disease, ulcerative colitis | Lowers the need for surgical intervention and reduces hospitalisations by preserving bowel health13,14 |
| Systemic lupus erythematosus | Prevents accelerated accumulation of damage, fatigue and increased mortality10 |
The role of general practitioners in polyautoimmunity: Identifying patients with the relevant symptoms and history for diagnostic testing
GPs are on the front line of patient care. By recognising the challenges patients face with time to diagnosis, GPs can help alleviate the distress and mistrust that many patients experience due to delays.
- Autoimmune thyroid diseases, including Hashimoto's thyroiditis and Graves' disease, belong to the most prevalent autoimmune diseases in the world and manifest through diverse symptoms such as fatigue, weight changes and mood disturbances.15 Polyautoimmunity is found in about 13.5% of patients with autoimmune thyroiditis with high frequencies of type 1 diabetes mellitus, autoimmune gastritis, rheumatoid arthritis, coeliac disease, vitiligo and pernicious anaemia.7
- Coeliac disease is a heavily underdiagnosed autoimmune condition and can present with gastrointestinal issues, anaemia and dermatitis herpetiformis.16 Studies indicate that coeliac disease can be present as a comorbidity in up to 12% of patients diagnosed with type 1 diabetes mellitus, Sjögren's syndrome, autoimmune thyroiditis and others.16
- Connective tissue diseases (CTDs), such as systemic lupus erythematosus, scleroderma and polymyositis, are systemic autoimmune diseases that can present with a broad range of symptoms, including joint pain, skin rashes and organ dysfunction.15 Polyautoimmunity is common among CTD patients and it is therefore highly likely for individuals with a CTD to meet the clinical criteria for at least one additional autoimmune disease. Common comorbidities in CTD patients include rheumatoid arthritis, autoimmune thyroiditis, antiphospholipid syndrome and autoimmune liver diseases.17
- Inflammatory bowel diseases (IBDs) are chronic autoimmune conditions with symptoms such as abdominal pain, diarrhoea and weight loss.15,18 IBD patients have a higher risk of developing other autoimmune diseases like coeliac disease, autoimmune hepatitis, type 1 diabetes mellitus, psoriasis and others.18,19
By recognising symptoms early, GPs can select appropriate diagnostic tools, such as autoantibody tests, to confirm the suspicion of autoimmune disease and support secondary care providers in identifying polyautoimmunity in their patients.5,10
Three tips for patient communication
Empathy
Acknowledge the patient's fears. Reassure them that their symptoms are being taken seriously. Empathy improves patient satisfaction, reduces anxiety, enhances outcomes and strengthens patient engagement.20
Education
Explain polyautoimmunity in simple terms. Discuss the potential for multiple autoimmune diseases and the importance of monitoring.
Managing expectations
Set realistic expectations about the diagnostic process and treatment pathway. Emphasise the importance of follow-up appointments and ongoing care.
Example of early GP intervention (fictional case): Consider a 24-year-old woman managing type 1 diabetes who presented with unexplained fatigue, abdominal pain and significant weight loss. Her vigilant GP, suspecting more than poor glycaemic control, ordered a test for anti-tissue transglutaminase antibodies (anti-tTG IgA) which revealed a high likelihood of hidden coeliac disease. This early detection by the GP allowed for prompt intervention, preventing complications such as malnutrition, osteoporosis and an increased risk of certain cancers.16,21,22
A gluten-free diet, which can be challenging, helped her overcome debilitating symptoms like fatigue and abdominal pain. With renewed energy, she could once again participate in family activities and social events. This change not only relieved her physical symptoms but also improved her mental well-being, allowing her to lead a more active and fulfilling life.
Learn more about this case study
Read the full case study to understand the critical role GPs play in identifying and managing polyautoimmunity, transforming patient outcomes through timely and preventive care.
Case finding and reducing time to diagnosis: One of the major challenges with autoimmune diseases is the frequent delay in diagnosis, which increases the risk of further damage due to disease progression.9,10,13,14,21 For patients, delayed diagnosis often means prolonged suffering, ongoing symptoms and in severe cases, further deterioration in quality of life.10,11,13,21 GPs can play a crucial role in case finding—actively looking for potential cases of polyautoimmunity in patients with existing autoimmune conditions.5,12,23
GPs can:
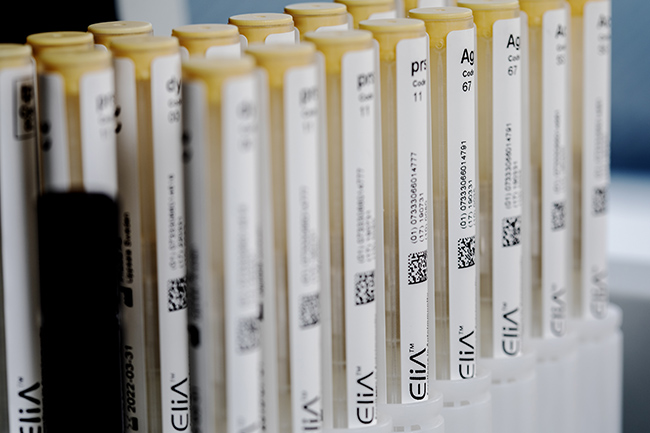
- Utilise comprehensive diagnostic tests such as EliA™ autoimmune diagnostics.
- Stay updated with the latest clinical guidelines and diagnostic criteria.
- Maintain a high index of suspicion for symptoms of additional autoimmune diseases in patients already diagnosed with one.
For instance, if a patient with autoimmune thyroid disease presents with symptoms of coeliac disease, timely testing can lead to a faster diagnosis and appropriate referral to a specialist.12,16 By doing so, GPs can significantly reduce the time to diagnosis, offering patients quicker relief and reducing the risk of long-term complications.
Providing answers and relief to patients: Autoimmune diseases can be life-altering and patients often experience a prolonged period of uncertainty and distress.2,10,21 In a recent study, in-depth interviews with patients living with coeliac disease revealed that delays in diagnosis not only decreased their physiological well-being but also led to psychological distress and mistrust in the healthcare system.21
In summary, although polyautoimmunity is a growing concern that negatively impacts patients' lives, it also represents an opportunity for GPs to make a profound impact on patient care. By approaching patients with empathy, staying up to date with clinical and diagnostic guidelines and utilising comprehensive diagnostic tools, GPs can help to reduce diagnostic delays, provide relief and ensure qualified referrals to improve patient outcomes.