This illustrative case study explores an example of a young man's, David, journey, demonstrating how cutting-edge allergy diagnostics helped manage his persistent allergic rhinitis symptoms. His story highlights the pivotal role of Thermo Fisher Scientific’s ImmunoCAPTM specific IgE test results in helping general practitioners identify and manage allergies with precision. Dive into the details and see the difference accurate allergy diagnostics can make in primary care.

Patient History
Personal history
David was previously diagnosed with seasonal allergic rhinitis at the age of 16. He first noticed his symptoms in May and they were at their worst in July. At the age of 18, he was diagnosed with mild depression.
Medication history
- Previously trialed intranasal antihistamines, which were ineffective at controlling his nasal symptoms
- Currently prescribed an antihistamine/corticosteroid combination intranasal spray
Examination, investigations and results
Examination
Whilst talking to David, his GP noticed that he had nasal speech and was frequently sniffing and rubbing his nose. Allergic shiners, discolored circles under the eyes, were observed upon close inspection of his face and internal examination of his nose revealed turbinate hypertrophy.
Examination and auscultation of David’s chest revealed no obvious abnormalities or stigmata of asthma.
Which of David’s symptoms are particularly suggestive of allergic rhinitis, as opposed to non-allergic rhinitis?
Manifestations of rhinitis, which are particularly suggestive of allergy, are:1
- Itchy nose and/or palate
- Sneezing
- Eye-related symptoms
Investigations
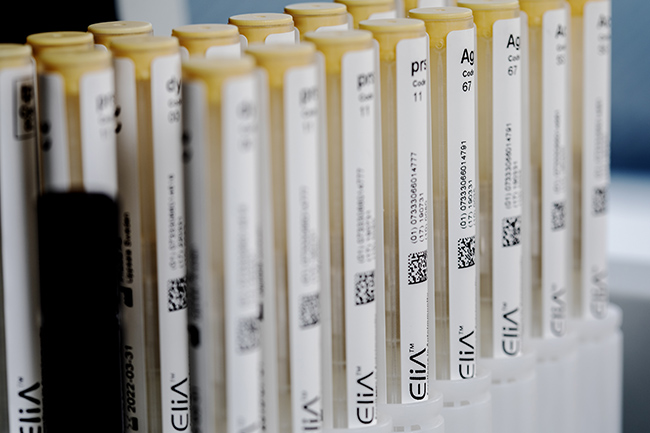
David’s GP decided to request a specific IgE blood test; Allergy blood tests are not affected by antihistamines and can be performed in patients who have recently taken them, such as David.2 The panel of allergens was selected based on David’s symptoms, age and local sensitisation patterns. As his symptoms usually begin in May and are at their worst in July, a range of allergens that typically present in spring/summer (including pollens and a fungus), were selected for testing.

ImmunoCAP™ specific IgE blood test results (kUA/L) |
||
Test* |
Type |
David’s results |
Timothy grass (g6) |
Whole allergen |
38 |
Silver birch (t3) |
Whole allergen |
<0.10 |
Common ragweed (w1) |
Whole allergen |
<0.10 |
Mugwort (w6) |
Whole allergen |
<0.10 |
Alternaria alternata (m6) |
Whole allergen |
<0.10 |
How could these specific IgE blood test results guide the GP’s management of David?
Specific IgE blood test results could guide the GP’s management of David in various ways, including:3,4
- Confirmation of his previous seasonal allergic rhinitis diagnosis
- Determination of appropriate pharmacotherapy and timing of therapy
- Guidance on local allergen avoidance strategies
- Consideration of allergen immunotherapy†
†Refer to specialists/allergists for allergen immunotherapy, if required.
Differential diagnosis
The results showed a significant IgE response to Timothy grass, confirming the previous diagnosis of seasonal allergic rhinitis. No other sensitisations were found, so allergies to birch pollen, ragweed, mugwort and Alternaria alternata can be ruled out.
Management
As Timothy grass is an outdoor allergen, it cannot be completely avoided.5 However, David could use the following techniques to help limit his exposure:5
- Check local pollen counts to anticipate grass pollen season and monitor pollen levels.
- Keep windows closed during pollen season.
- Take a shower, wash hair, and change clothing after working or playing outdoors.
Information gained from specific IgE blood tests can be an important factor in better pharmacotherapy management. For example, commencing therapy just before the start of the local grass pollen season could maximise treatment effectiveness for David.3
Allergen immunotherapy (AIT) is the only potentially disease-modifying option for the treatment of allergies7 and is usually initiated by allergy specialists.8 Appropriate AIT can prevent the development of asthma9 and, in patients with comorbid asthma, improve symptom control.10 David’s GP decided to refer him to an allergy specialist for selection of AIT.
*The following products are included in the ImmunoCAP™ blood test portfolio:
- ImmunoCAP Allergen g6, Timothy
- ImmunoCAP Allergen t3, Common silver birch
- ImmunoCAP Allergen w1, Common ragweed
- ImmunoCAP Allergen w6, Mugwort
- ImmunoCAP Allergen m6, Alternaria alternata
IgE: immunoglobulin E; kUA/L: allergen-specific kilo units per litre
Conclusion
David's steps from suffering to relief highlight the essential role of precise allergy diagnostics and customized treatment plans. With Thermo Fisher Scientific’s ImmunoCAP specific IgE test solutions, his general practitioner was provided with accurate results to guide personalized care that significantly enhanced David’s quality of life.
The people, places and events depicted in these case studies and photographs do not represent actual patients, nor are they affiliated in any way with Thermo Fisher Scientific.
Put us to the test and see how our trusted diagnostic solutions can aid in the diagnosis of allergy and help you deliver the best possible care for your patients.