Egg allergy diagnosis:
a step-by-step guide
About egg allergy
Accurate diagnosis of food allergy is essential for personalised patient management,1 including avoidance of unnecessary dietary restrictions and prevention of life-threatening reactions.2 Egg is one of the most common food allergy sources, particularly in infants and children.1 The prevalence of egg allergy in children is estimated to be around 0.5-2.5 percent.3
Read through this evidence-based guide to learn how to accurately diagnose egg allergy in clinical practice.
Steps 1-2: primary care
1. Medical history and physical examination
A detailed clinical history is crucial but not sufficient alone to make a diagnosis of egg allergy. The goals of the clinical history are to:4,5
- Establish the likelihood of egg allergy (or other allergy) as a diagnosis
- Identify whether an IgE or non-IgE mechanism is involved
- Guide appropriate immunological tests
Egg allergy is most commonly IgE-mediated, and usually presents as an immediate-type reaction (within minutes to hours after ingestion).
IgE-mediated egg allergy:6
- Typically causes cutaneous symptoms: urticaria or angio-oedema
- May involve the gastrointestinal and respiratory systems
- Is unpredictable in severity, and may vary between episodes
- Can cause anaphylaxis*
*Anaphylaxis or shock-like symptoms are clear indications for a referral to an allergy specialist.
The physical examination should thoroughly assess nutritional status and growth, especially in children, as well as associated atopic diseases such as atopic dermatitis and asthma.5
- Atopic dermatitis: flares may be seen in infants and young children with egg allergy; delayed reactions (6-48 hours following ingestion) are suggestive of non-IgE-mediated reactions.6
- Asthma: adults with IgE-mediated egg allergy who are frequently exposed to aerosolised egg (e.g., bakery workers) may develop occupational asthma.6
Gastroenteropathies, such as allergic eosinophilic oesophagitis, are occasionally seen in children with egg allergy, and are mediated by a combination of IgE and non-IgE immunological processes.6
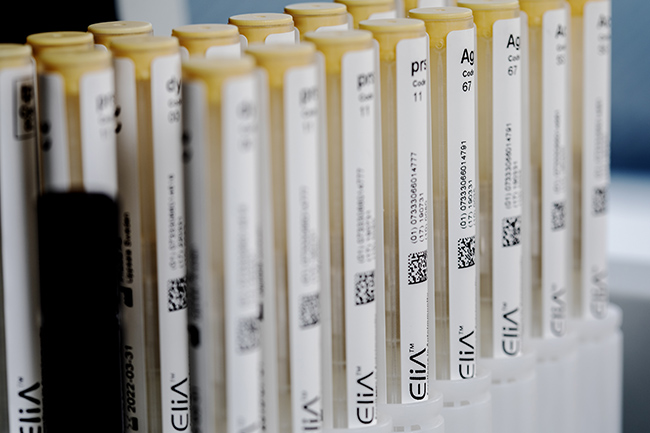
2. Laboratory tests such as specific IgE blood tests
If the patient’s history indicates IgE-mediated allergy, specific IgE blood tests can assist in the diagnosis.7,8 Specific IgE blood tests can be performed at any age and use validated assays to quantify allergen-specific IgE levels in the serum.7 Firstly, a test for a specific IgE response to the whole allergen (egg) should be performed.8
Interpretation of whole-allergen specific IgE blood test results
- Results should always be interpreted in the context of the patient’s clinical history.6
- The presence of a specific IgE response to the whole allergen indicates a sensitisation to egg, and an associated IgE-mediated immunological process.8
- The higher the antibody titre, the greater the probability of having egg allergy.9
Whole-allergen tests predict the likelihood of egg allergy but are not predictive of reactivity to cooked egg. After testing for a specific IgE response to whole allergen, egg allergen component tests can help evaluate reactivity to cooked egg and provide further information on the likelihood of allergy persistence.6,8
Assessment of specific IgE responses to the following components (proteins) could help pinpoint the diagnosis and guide the management of patients with egg allergy:8
- Ovomucoid (f233 / Gal d 1)
- Ovalbumin (f232 / Gal d 2)
- Conalbumin (f323 / nGal d 3)
- Lysozyme (k208 / Gal d 4)
As ovomucoid is more resistant than other proteins to heat denaturation, patients with high levels of ovomucoid-specific IgE are likely to react to cooked egg. Such patients should therefore avoid consumption of all forms of egg. Patients who test negative for ovomucoid-specific IgE may be able to tolerate cooked egg.8
70 percent of children with egg allergy do not react to egg in baked products.10
Consider using allergen component blood tests to identify these patients.8
Steps 3-6: secondary care
3. Diagnostic elimination diet
If relevant symptoms are present and egg allergy is likely, a diagnostic elimination diet should be initiated. Egg should be strictly excluded from the patient’s diet for a limited period.5
The duration of the elimination diet should be kept as short as possible whilst being long enough to judge whether clinical symptoms resolve or stabilise (usually 2-4 weeks for IgE-mediated symptoms). Symptoms should be carefully monitored:5
- If symptoms significantly improve, the elimination diet should be continued until the oral food challenge (OFC) is performed (see step 4).
- If symptoms do not significantly improve, egg allergy is unlikely (but consider the possibility of inadvertent egg consumption or multiple sensitisations).
4. Oral food challenge
Sometimes the clinical history and specific IgE blood test results are strongly suggestive of an egg allergy, but often an OFC with egg is necessary to confirm the diagnosis. The presence or absence of a symptomatic response will demonstrate allergy or tolerance, respectively.5
OFCs should be performed in a specialist setting with rapid emergency support available; for patients deemed by their healthcare provider to be at medium-to-high risk of having a severe reaction, intensive care support must also be immediately available.5
5. Strict exclusion of egg from the diet
When a diagnosis of egg allergy has been confirmed, avoidance of egg-containing food should form the basis of the management strategy.11 As egg is found in a wide range of food products, dietary avoidance can be challenging and pose significant quality-of-life concerns.6 Elimination diets in young children may result in poor nutrition, meaning growth parameters should be closely monitored.11
Based on allergen-component blood test results, patients may be able to tolerate extensively heated egg.11 Dietary inclusion of products containing extensively heated egg may accelerate development of tolerance to unheated egg.6
6. Re-evaluation at 6-12 months
Patients should be re-evaluated at around 6-12 months, to avoid continuing the restrictive exclusion diet for an unnecessarily long time. Repeated specific IgE blood tests can be helpful to:5
- Determine whether sensitisation is decreasing (common in egg allergy)
- Identify associated allergies
IgE: immunoglobulin E
- De Martinis M, Sirufo M M et al. New perspectives in food allergy. Int J Mol Sci 2020;21(4)
- Kattan J D, Sicherer S H. Optimizing the diagnosis of food allergy. Immunol Allergy Clin North Am 2015;35(1):61-76
- Rona R J, Keil T et al. The prevalence of food allergy: a meta-analysis. J Allergy Clin Immunol 2007;120(3):638-646
- Turnbull J L, Adams H N, Gorard D A. Review article: the diagnosis and management of food allergy and food intolerances. Aliment Pharmacol Ther 2015;41(1):3-25
- Muraro A, Werfel T et al. EAACI food allergy and anaphylaxis guidelines: diagnosis and management of food allergy. Allergy 2014;69(8):1008-1025
- Caubet J C, Wang J. Current understanding of egg allergy. Pediatr Clin North Am 2011;58(2):427-443, xi
- Eigenmann P A, Atanaskovic-Markovic M et al. Testing children for allergies: why, how, who and when: an updated statement of the European Academy of Allergy and Clinical Immunology (EAACI) Section on Pediatrics and the EAACI-Clemens von Pirquet Foundation. Pediatr Allergy Immunol 2013;24(2):195-209
- Matricardi P M, Kleine-Tebbe J et al. EAACI molecular allergology user's guide. Pediatr Allergy Immunol 2016;27 Suppl 23:1-250
- Soderstrom L, Kober A et al. A further evaluation of the clinical use of specific IgE antibody testing in allergic diseases. Allergy 2003;58(9):921-928
- Lemon-Mule H, Sampson H A et al. Immunologic changes in children with egg allergy ingesting extensively heated egg. J Allergy Clin Immunol 2008;122(5):977-983 e971
- Heine R G, Laske N, Hill D J. The diagnosis and management of egg allergy. Curr Allergy Asthma Rep 2006;6(2):145-152

Legal manufacturer: Phadia AB.
Before you proceed ...
We noticed you may be visiting a version of our website that doesn’t match your current location. Would you like to view content based on your region?
Talk with us
Interested in utilizing our solutions in your laboratory or healthcare practice?
This form is dedicated to healthcare and laboratory professionals who work within medical laboratories, private practices, health systems, and the like.
By clicking "continue with form" you are confirming that you work within a healthcare or laboratory space.
Not a lab professional or clinician but interested in diagnostic testing for allergies?
Visit Allergy InsiderChoose your preferred language
Please note: By selecting a different language, you are choosing to view another site. Product availability and indications may vary from what is approved in your region.