Alpha-Gal syndrome, a trigger of red meat allergy
Alpha-Gal syndrome, a red meat allergy, is triggered by IgE antibodies targeting galactose-alpha-1,3-galactose known as “alpha-Gal” found in the meats of non-primate mammals. Tick bites are the primary carrier for this sensitization. Recognizing a potential connection to tick bites can significantly aid the diagnostic process. 1,3

Alpha-Gal clinical manifestations
Alpha-Gal syndrome commonly appears in adolescents and adults, as symptoms range from unexpected urticaria (itchy rash and hives) to gastrointestinal problems (diarrhoea), and, in severe cases, anaphylaxis. Symptoms typically appear 3-6 hours after consuming red meat (like beef, pork, lamb or innards).1-4
Often misdiagnosed as irritable bowel syndrome, there is a significant amount of underdiagnosis, with about 80% of patients experiencing delays of over seven years in receiving an accurate diagnosis. Fortunately, efforts in heightened awareness and enhanced diagnostic methods are fostering a positive shift. This progress holds promise for shorter diagnosis times, providing an improvement in recognizing and managing alpha-Gal allergies.5
The risk and severity of reactions in alpha-Gal syndrome are influenced by the oligosaccharide quantity in food, drugs or therapeutics. Administration route matters, as intravenous exposure triggers rapid reactions, while oral ingestion leads to delayed onset.
Diagnostic approaches
In the case of suspected mammalian meat allergy, a detailed clinical history focusing on predisposing factors such as tick bites, meat consumption and the onset of symptoms, as well as potential cofactors like alcohol consumption, physical activity and the use of nonsteroidal anti-inflammatory drugs, is essential due to the varying reactions among patients.2,7
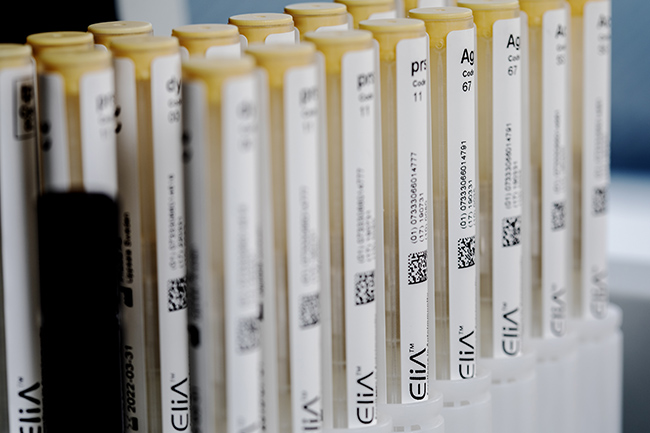
The employment of specific IgE blood tests, such as the ImmunoCAPTM Specific IgE test, enhances this analysis by offering a more precise and reliable diagnosis. This approach enables healthcare professionals to develop tailored and effective care strategies for each patient.6,8
In a typical alpha-Gal allergic patient:
- Diagnosis is supported by IgE to several mammalian meats: pork, beef and lamb.9
- IgE levels against alpha-Gal are higher compared to IgE against mammalian meats.9, 10
Management consideration
Specific IgE tests results should be interpreted along with patient history, symptoms and physical examination to aid in diagnosis and management plan development.4,6
Learn more about alpha-Gal and ImmunoCAP Specific IgE tests.
Beyond alpha-Gal syndrome: Pork cat syndrome & cow's milk allergen cross-reactivity
It is also important to be aware that there are other types of IgE-mediated meat allergies, such as:
- Pork-cat syndrome: a rare reaction to pork in individuals sensitized to cat serum albumin, due to cross-reactivity between serum albumins. This involves an immediate IgE response. Diagnosis includes specific IgE tests for pork, cat and cat serum albumin (Fel d 2).11
- Cow's milk allergen cross-reactivity: 10-20% of children with cow milk allergy may have a cross-allergy to beef or veal due to serum albumin from cow's milk (Bos d 6).12, 13
Specific IgE blood testing can help narrow your differential diagnosis.
You have the power to make a difference.
* Full name of products: ImmunoCAP Allergen e1, Cat dander; ImmunoCAP Allergen e220, component rFel d 2, Cat serum albumin; ImmunoCAP Allergen e204, component nBos d 6, Bovin Serum Albumin